| MeSH term | MeSH ID | Detail |
|---|---|---|
| Hemolysis | D006461 | 131 associated lipids |
| Uremia | D014511 | 33 associated lipids |
| Colitis, Ulcerative | D003093 | 24 associated lipids |
| Stomach Ulcer | D013276 | 75 associated lipids |
| Kidney Failure, Chronic | D007676 | 51 associated lipids |
| Nocardia Infections | D009617 | 6 associated lipids |
| Diarrhea | D003967 | 32 associated lipids |
| Diabetes Mellitus | D003920 | 90 associated lipids |
| Graft Occlusion, Vascular | D006083 | 11 associated lipids |
| Hypercalcemia | D006934 | 13 associated lipids |
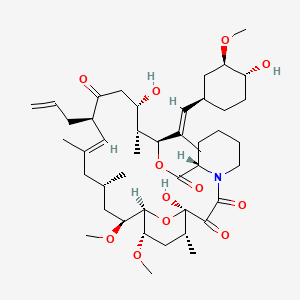
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Chen ZS et al. | Early steroid withdrawal after liver transplantation for hepatocellular carcinoma. | 2007 | World J. Gastroenterol. | pmid:17876900 |
| Song JL et al. | Minimizing tacrolimus decreases the risk of new-onset diabetes mellitus after liver transplantation. | 2016 | World J. Gastroenterol. | pmid:26877618 |
| Li DW et al. | Risk factors for new onset diabetes mellitus after liver transplantation: A meta-analysis. | 2015 | World J. Gastroenterol. | pmid:26034369 |
| Provenzani A et al. | Pharmacogenetic considerations for optimizing tacrolimus dosing in liver and kidney transplant patients. | 2013 | World J. Gastroenterol. | pmid:24409044 |
| Guo YW et al. | Successful treatment of ileal ulcers caused by immunosuppressants in two organ transplant recipients. | 2016 | World J. Gastroenterol. | pmid:27350740 |
| Jia JJ et al. | ''Minimizing tacrolimus'' strategy and long-term survival after liver transplantation. | 2014 | World J. Gastroenterol. | pmid:25170223 |
| Hilgard P et al. | Cyclosporine versus tacrolimus in patients with HCV infection after liver transplantation: effects on virus replication and recurrent hepatitis. | 2006 | World J. Gastroenterol. | pmid:16521181 |
| Eshraghian A et al. | Post-transplant lymphoproliferative disorder after liver transplantation: Incidence, long-term survival and impact of serum tacrolimus level. | 2017 | World J. Gastroenterol. | pmid:28275302 |
| Jiang JW et al. | Optimal immunosuppressor induces stable gut microbiota after liver transplantation. | 2018 | World J. Gastroenterol. | pmid:30228781 |
| Wu SY et al. | Comprehensive risk assessment for early neurologic complications after liver transplantation. | 2016 | World J. Gastroenterol. | pmid:27350733 |
| Liu C et al. | Cyclosporine A, FK-506, 40-0-[2-hydroxyethyl]rapamycin and mycophenolate mofetil inhibit proliferation of human intrahepatic biliary epithelial cells in vitro. | 2005 | World J. Gastroenterol. | pmid:16437685 |
| Kawakami K et al. | Effects of oral tacrolimus as a rapid induction therapy in ulcerative colitis. | 2015 | World J. Gastroenterol. | pmid:25684955 |
| Okan G et al. | Vanishing bile duct and Stevens-Johnson syndrome associated with ciprofloxacin treated with tacrolimus. | 2008 | World J. Gastroenterol. | pmid:18698687 |
| Larsen FS et al. | Low-dose tacrolimus ameliorates liver inflammation and fibrosis in steroid refractory autoimmune hepatitis. | 2007 | World J. Gastroenterol. | pmid:17589903 |
| Indriolo A and Ravelli P | Clinical management of inflammatory bowel disease in the organ recipient. | 2014 | World J. Gastroenterol. | pmid:24707135 |
| Buchholz BM et al. | Role of colectomy in preventing recurrent primary sclerosing cholangitis in liver transplant recipients. | 2018 | World J. Gastroenterol. | pmid:30065563 |
| Shen T et al. | Reversible sinusoidal obstruction syndrome associated with tacrolimus following liver transplantation. | 2015 | World J. Gastroenterol. | pmid:26034381 |
| Jordan ML et al. | The use of tacrolimus in renal transplantation. | 1996 | World J Urol | pmid:8873438 |
| Schlosser K et al. | Surgical treatment of tertiary hyperparathyroidism: the choice of procedure matters! | 2007 | World J Surg | pmid:17665243 |
| Ramakant P and Agarwal G | Surgical treatment of tertiary hyperparathyroidism: the choice of procedure matters: surgical management of tertiary hyperparathyroidism: an enigma. | 2008 | World J Surg | pmid:18404286 |