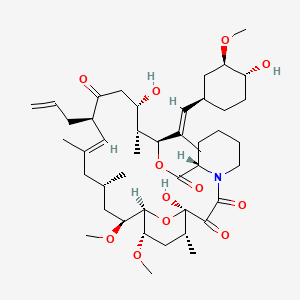
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- Am. J. Physiol. Renal Physiol. (1)
- Drug Metab. Dispos. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Finn L et al. | Epstein-Barr virus infections in children after transplantation of the small intestine. | 1998 | Am. J. Surg. Pathol. | pmid:9500771 |
| Randhawa PS et al. | The histopathological changes associated with allograft rejection and drug toxicity in renal transplant recipients maintained on FK506. Clinical significance and comparison with cyclosporine. | 1993 | Am. J. Surg. Pathol. | pmid:7680544 |
| Minervini MI et al. | Acute renal allograft rejection with severe tubulitis (Banff 1997 grade IB). | 2000 | Am. J. Surg. Pathol. | pmid:10757402 |
| Randhawa PS et al. | Microvascular changes in renal allografts associated with FK506 (Tacrolimus) therapy. | 1996 | Am. J. Surg. Pathol. | pmid:8772784 |
| Campbell PM et al. | Pretransplant HLA antibodies are associated with reduced graft survival after clinical islet transplantation. | 2007 | Am. J. Transplant. | pmid:17456201 |
| Boudjema K et al. | Reduced-dose tacrolimus with mycophenolate mofetil vs. standard-dose tacrolimus in liver transplantation: a randomized study. | 2011 | Am. J. Transplant. | pmid:21466650 |
| Knechtle SJ | Guidance for liver transplant immunosuppression. | 2011 | Am. J. Transplant. | pmid:21466652 |
| Gupta G et al. | Safe Conversion From Tacrolimus to Belatacept in High Immunologic Risk Kidney Transplant Recipients With Allograft Dysfunction. | 2015 | Am. J. Transplant. | pmid:25988397 |
| Silva HT et al. | Planned randomized conversion from tacrolimus to sirolimus-based immunosuppressive regimen in de novo kidney transplant recipients. | 2013 | Am. J. Transplant. | pmid:24266969 |
| Ricciardelli I et al. | Rapid generation of EBV-specific cytotoxic T lymphocytes resistant to calcineurin inhibitors for adoptive immunotherapy. | 2013 | Am. J. Transplant. | pmid:24266973 |
| Suszynski TM et al. | Prospective randomized trial of maintenance immunosuppression with rapid discontinuation of prednisone in adult kidney transplantation. | 2013 | Am. J. Transplant. | pmid:23432755 |
| Damon C et al. | Predictive Modeling of Tacrolimus Dose Requirement Based on High-Throughput Genetic Screening. | 2017 | Am. J. Transplant. | pmid:27597269 |
| Ferguson R et al. | Immunosuppression with belatacept-based, corticosteroid-avoiding regimens in de novo kidney transplant recipients. | 2011 | Am. J. Transplant. | pmid:21114656 |
| McKenna G and Trotter JF | Does early (CNI) conversion lead to eternal (renal) salvation? | 2010 | Am. J. Transplant. | pmid:20928938 |
| Shuker N et al. | A Randomized Controlled Trial Comparing the Efficacy of Cyp3a5 Genotype-Based With Body-Weight-Based Tacrolimus Dosing After Living Donor Kidney Transplantation. | 2016 | Am. J. Transplant. | pmid:26714287 |
| Forns X and Navasa M | Cyclosporine A or tacrolimus for hepatitis C recurrence? An old debate. | 2011 | Am. J. Transplant. | pmid:21797970 |
| Arnold R et al. | Association between calcineurin inhibitor treatment and peripheral nerve dysfunction in renal transplant recipients. | 2013 | Am. J. Transplant. | pmid:23841745 |
| Hirsch HH et al. | BK Polyomavirus Replication in Renal Tubular Epithelial Cells Is Inhibited by Sirolimus, but Activated by Tacrolimus Through a Pathway Involving FKBP-12. | 2016 | Am. J. Transplant. | pmid:26639422 |
| Bohl DL et al. | Donor origin of BK virus in renal transplantation and role of HLA C7 in susceptibility to sustained BK viremia. | 2005 | Am. J. Transplant. | pmid:16095500 |
| Kasahara M et al. | Living-donor liver transplantation for hepatoblastoma. | 2005 | Am. J. Transplant. | pmid:16095502 |
| Madeleine MM et al. | HPV-related cancers after solid organ transplantation in the United States. | 2013 | Am. J. Transplant. | pmid:24119294 |
| Lemahieu WP et al. | CYP3A4 and P-glycoprotein activity in healthy controls and transplant patients on cyclosporin vs. tacrolimus vs. sirolimus. | 2004 | Am. J. Transplant. | pmid:15307840 |
| Bressollette-Bodin C et al. | A prospective longitudinal study of BK virus infection in 104 renal transplant recipients. | 2005 | Am. J. Transplant. | pmid:15996241 |
| Augustine JJ et al. | Pre-transplant IFN-gamma ELISPOTs are associated with post-transplant renal function in African American renal transplant recipients. | 2005 | Am. J. Transplant. | pmid:15996247 |
| Filler G et al. | Adding sirolimus to tacrolimus-based immunosuppression in pediatric renal transplant recipients reduces tacrolimus exposure. | 2005 | Am. J. Transplant. | pmid:15996252 |
| Froud T et al. | Islet transplantation in type 1 diabetes mellitus using cultured islets and steroid-free immunosuppression: Miami experience. | 2005 | Am. J. Transplant. | pmid:15996257 |
| Chodoff L and Hamberg KJ | Response to 'Different preparations of tacrolimus and medication errors'. | 2009 | Am. J. Transplant. | pmid:19392982 |
| Luther P and Baldwin D | Pioglitazone in the management of diabetes mellitus after transplantation. | 2004 | Am. J. Transplant. | pmid:15575920 |
| Cherukuri A et al. | An analysis of lymphocyte phenotype after steroid avoidance with either alemtuzumab or basiliximab induction in renal transplantation. | 2012 | Am. J. Transplant. | pmid:22390816 |
| Dahm F et al. | Conversion from cyclosporine to tacrolimus improves quality-of-life indices, renal graft function and cardiovascular risk profile. | 2004 | Am. J. Transplant. | pmid:15575921 |
| Pascher A et al. | Protein kinase C inhibitor sotrastaurin in de novo liver transplant recipients: a randomized phase II trial. | 2015 | Am. J. Transplant. | pmid:25677074 |
| Barth RN et al. | Vascularized bone marrow-based immunosuppression inhibits rejection of vascularized composite allografts in nonhuman primates. | 2011 | Am. J. Transplant. | pmid:21668624 |
| Guirado L et al. | Efficacy and safety of conversion from twice-daily to once-daily tacrolimus in a large cohort of stable kidney transplant recipients. | 2011 | Am. J. Transplant. | pmid:21668633 |
| Flechner SM et al. | The ORION study: comparison of two sirolimus-based regimens versus tacrolimus and mycophenolate mofetil in renal allograft recipients. | 2011 | Am. J. Transplant. | pmid:21668635 |
| Grenda R et al. | A randomized trial to assess the impact of early steroid withdrawal on growth in pediatric renal transplantation: the TWIST study. | 2010 | Am. J. Transplant. | pmid:20420639 |
| Montgomery SP et al. | Efficacy and toxicity of a protocol using sirolimus, tacrolimus and daclizumab in a nonhuman primate renal allotransplant model. | 2002 | Am. J. Transplant. | pmid:12118862 |
| van Hooff JP et al. | Glucose metabolic disorder after transplantation. | 2007 | Am. J. Transplant. | pmid:17511670 |
| Silva HT et al. | One-year results with extended-release tacrolimus/MMF, tacrolimus/MMF and cyclosporine/MMF in de novo kidney transplant recipients. | 2007 | Am. J. Transplant. | pmid:17217442 |
| Heffron TG et al. | Once-daily tacrolimus extended-release formulation: 1-year post-conversion in stable pediatric liver transplant recipients. | 2007 | Am. J. Transplant. | pmid:17511684 |
| Moench C et al. | Tacrolimus monotherapy without steroids after liver transplantation--a prospective randomized double-blinded placebo-controlled trial. | 2007 | Am. J. Transplant. | pmid:17511685 |
| Patlolla V et al. | Efficacy of anti-IL-2 receptor antibodies compared to no induction and to antilymphocyte antibodies in renal transplantation. | 2007 | Am. J. Transplant. | pmid:17564638 |
| Nijhoff MF et al. | Glycemic Stability Through Islet-After-Kidney Transplantation Using an Alemtuzumab-Based Induction Regimen and Long-Term Triple-Maintenance Immunosuppression. | 2016 | Am. J. Transplant. | pmid:26288226 |
| Toso C et al. | Sequential kidney/islet transplantation: efficacy and safety assessment of a steroid-free immunosuppression protocol. | 2006 | Am. J. Transplant. | pmid:16611343 |
| Lacaille F et al. | Severe dysimmune cytopenia in children treated with tacrolimus after organ transplantation. | 2006 | Am. J. Transplant. | pmid:16611346 |
| Chamie K et al. | The effect of sirolimus on prostate-specific antigen (PSA) levels in male renal transplant recipients without prostate cancer. | 2008 | Am. J. Transplant. | pmid:18853950 |
| Lefaucheur C et al. | Renal histopathological lesions after lung transplantation in patients with cystic fibrosis. | 2008 | Am. J. Transplant. | pmid:18671673 |
| Pech T et al. | Intestinal regeneration, residual function and immunological priming following rescue therapy after rat small bowel transplantation. | 2012 | Am. J. Transplant. | pmid:22974463 |
| McDonald RA et al. | Incidence of PTLD in pediatric renal transplant recipients receiving basiliximab, calcineurin inhibitor, sirolimus and steroids. | 2008 | Am. J. Transplant. | pmid:18416737 |
| Brennan DC et al. | Incidence of BK with tacrolimus versus cyclosporine and impact of preemptive immunosuppression reduction. | 2005 | Am. J. Transplant. | pmid:15707414 |
| Chhabra D et al. | Impact of calcineurin-inhibitor conversion to mTOR inhibitor on renal allograft function in a prednisone-free regimen. | 2013 | Am. J. Transplant. | pmid:24007570 |