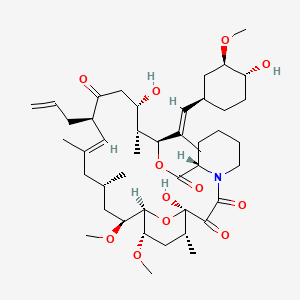
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- Am. J. Physiol. Renal Physiol. (1)
- Drug Metab. Dispos. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| pmid:8615615 | ||||
| Payabvash S et al. | Cerebellar superficial siderosis of chronic subarachnoid hemorrhage in a patient with Tacrolimus-associated posterior reversible encephalopathy. | J Postgrad Med | pmid:25370549 | |
| Akoglu H et al. | Relationship between hemorheology and endothelial dysfunction in renal transplant patients receiving calcineurin inhibitors. | J. Nephrol. | pmid:23147686 | |
| Omland SH and Gniadecki R | Psoriasis inversa: A separate identity or a variant of psoriasis vulgaris? | Clin. Dermatol. | pmid:26051061 | |
| pmid:19200227 | ||||
| Chia BK and Tey HL | Systematic review on the efficacy, safety, and cost-effectiveness of topical calcineurin inhibitors in atopic dermatitis. | Dermatitis | pmid:25984688 | |
| Luger T et al. | Recommendations for pimecrolimus 1% cream in the treatment of mild-to-moderate atopic dermatitis: from medical needs to a new treatment algorithm. | Eur J Dermatol | pmid:24185493 | |
| Park J et al. | Persistent generalized lichen nitidus successfully treated with 0.03% tacrolimus ointment. | Eur J Dermatol | pmid:24184632 | |
| Fernández C et al. | Kidney transplantation from HLA-incompatible live donors: Efficiency and outcome of 32 patients after desensitisation. | Nefrologia | pmid:28734583 | |
| Menéndez Valladares P et al. | [Increased lipoprotein(a) in a paediatric patient associated with nephrotic syndrome]. | Clin Investig Arterioscler | pmid:27623226 | |
| Yigitaslan S et al. | The Effect of P-Glycoprotein Inhibition and Activation on the Absorption and Serum Levels of Cyclosporine and Tacrolimus in Rats. | Adv Clin Exp Med | pmid:27627555 | |
| Kathuria S et al. | Segmental vitiligo: a randomized controlled trial to evaluate efficacy and safety of 0.1% tacrolimus ointment vs 0.05% fluticasone propionate cream. | Indian J Dermatol Venereol Leprol | pmid:22199063 | |
| Jefferson J et al. | Follicular Mucinosis in a Male Adolescent with a History of Acute Myelogenous Leukemia and Graft-versus-Host Disease. | Pediatr Dermatol | pmid:26645410 | |
| Sarvary E et al. | De novo Prograf versus de novo Advagraf: are trough level profile curves similar? | Transplant. Proc. | pmid:25131131 | |
| Borda B et al. | Early histopathological changes in new-onset diabetes after kidney transplantation. | Transplant. Proc. | pmid:25131129 | |
| Porubsky M et al. | Excellent outcomes can be achieved in young pancreas transplant alone recipients by addition of sirolimus to maintenance immunosuppression regimen. | Transplant. Proc. | pmid:25131074 | |
| Tulaci KG et al. | The effect of tacrolimus on facial nerve injury: Histopathological findings in a rabbit model. | Am J Otolaryngol | pmid:27465503 | |
| Liu JY et al. | Tacrolimus Versus Cyclosporine as Primary Immunosuppressant After Renal Transplantation: A Meta-Analysis and Economics Evaluation. | Am J Ther | pmid:25299636 | |
| pmid:9123014 | ||||
| Alokaily F et al. | Takayasu's arteritis and liver transplantation: Association and implications. | Saudi J Gastroenterol | pmid:26458863 | |
| Haroon N et al. | Tacrolimus Toxicity With Minimal Clinical Manifestations: A Case Report and Literature Review. | Am J Ther | pmid:25730156 | |
| Krzyżowska K et al. | No Significant Influence of Reduced Initial Tacrolimus Dose on Risk of Underdosing and Early Graft Function in Older and Overweight Kidney Transplant Recipients. | Transplant. Proc. | pmid:30056895 | |
| Zmonarski S et al. | Expression of PBMC TLR4 in Renal Graft Recipients Who Experienced Delayed Graft Function Reflects Dynamic Balance Between Blood and Tissue Compartments and Helps Select a Problematic Patient. | Transplant. Proc. | pmid:30056893 | |
| Zulim LFDC et al. | Comparison of the efficacy of 0.03% tacrolimus eye drops diluted in olive oil and linseed oil for the treatment of keratoconjunctivitis sicca in dogs. | Arq Bras Oftalmol | pmid:29995121 | |
| Kim K et al. | Everolimus-Induced Systemic Serositis After Simultaneous Liver and Kidney Transplantation: A Case Report. | Transplant. Proc. | pmid:28104132 | |
| Yamamoto T et al. | Efficacy of Eculizumab Therapy for Atypical Hemolytic Uremic Syndrome Recurrence and Antibody-Mediated Rejection Progress After Renal Transplantation With Preformed Donor-Specific Antibodies: Case Report. | Transplant. Proc. | pmid:28104125 | |
| Ülkümen PK et al. | Annular lichenoid dermatitis of youth in a 15-year-old boy: Topical tacrolimus as a treatment option. | Indian J Dermatol Venereol Leprol | pmid:27279324 | |
| Takahashi Y et al. | Pharmacokinetic Profile of Twice- and Once-daily Tacrolimus in Pediatric Kidney Transplant Recipients. | Transplant. Proc. | pmid:28104153 | |
| Shi Y et al. | Comparison of Mizoribine and Mycophenolate Mofetil With a Tacrolimus-Based Immunosuppressive Regimen in Living-Donor Kidney Transplantation Recipients: A Retrospective Study in China. | Transplant. Proc. | pmid:28104150 | |
| Pan D et al. | Tacrolimus-associated Diffuse Gastrointestinal Ulcerations and Pathergy: A Case Report. | Transplant. Proc. | pmid:28104141 | |
| Ash MM and Jolly PS | A Case Report of the Resolution of Multiple Recalcitrant Verrucae in a Renal Transplant Recipient After a Mycophenolate Mofetil Dose Reduction. | Transplant. Proc. | pmid:28104140 | |
| Nayeri A et al. | Acute Calcineurin Inhibitor Nephrotoxicity Secondary to Turmeric Intake: A Case Report. | Transplant. Proc. | pmid:28104136 | |
| Dedhia P et al. | Eculizumab and Belatacept for De Novo Atypical Hemolytic Uremic Syndrome Associated With CFHR3-CFHR1 Deletion in a Kidney Transplant Recipient: A Case Report. | Transplant. Proc. | pmid:28104134 | |
| Zhang J et al. | Chemotherapy for De Novo Gastric Adenocarcinoma After Deceased Orthotopic Liver Transplantation: A Case Report. | Transplant. Proc. | pmid:28104131 | |
| Britto-Williams P and Pansare M | Management of chronic idiopathic urticaria in childhood: are we on the same page? | J Allergy Clin Immunol Pract | pmid:24565627 | |
| Nojima M et al. | Immunosuppression Modification by Everolimus With Minimization of Calcineurin Inhibitors Recovers Kidney Graft Function Even in Patients With Very Late Conversion and Also With Poor Graft Function. | Transplant. Proc. | pmid:28104155 | |
| Ishida S et al. | Calcineurin Inhibitor-Induced Pain Syndrome in ABO-Incompatible Living Kidney Transplantation: A Case Report. | Transplant. Proc. | pmid:28104127 | |
| Liu JY et al. | Sirolimus Versus Tacrolimus as Primary Immunosuppressant After Renal Transplantation: A Meta-Analysis and Economics Evaluation. | Am J Ther | pmid:25569597 | |
| Norero B et al. | Â Conversion to mycophenolate mofetil monotherapy in liver recipients: Calcineurin inhibitor levels are key. | Ann Hepatol | pmid:28051798 | |
| Hirata Y et al. | Antibody Drug Treatment for Steroid-Resistant Rejection After Pediatric Living Donor Liver Transplantation: A Single-Center Experience. | Transplant. Proc. | pmid:29407332 | |
| Back JH et al. | Antiproteinuric Effects of Green Tea Extract on Tacrolimus-Induced Nephrotoxicity in Mice. | Transplant. Proc. | pmid:26293093 | |
| Shingaki S et al. | Graft-versus-host Disease-free, Relapse-free Survival After HLA-identical Sibling Peripheral Blood Stem Cell Transplantation With Tacrolimus-based Graft-versus-host Disease Prophylaxis in Japanese Patients. | Transplant. Proc. | pmid:29407317 | |
| Kim SH et al. | Outcomes of Early Conversion From Prograf to Generic Tacrolimus in Adult Living Donor Liver Transplant Recipients. | Transplant. Proc. | pmid:26293073 | |
| Falconer SJ et al. | Early or Late Conversion From Tac-BD to Tac-BD in Renal Transplantation: When is the Right Time? | Transplant. Proc. | pmid:26293044 | |
| Dall'Agnol DJ et al. | Effects of immunosuppressive drugs on gastrointestinal transit of rats: effects of tacrolimus, cyclosporine, and prednisone. | Transplant. Proc. | pmid:25131057 | |
| Mori F et al. | Increase of natural killer cells in children with liver transplantation-acquired food allergy. | Allergol Immunopathol (Madr) | pmid:29456038 | |
| pmid:28422431 | ||||
| Yousuf Bhat Z et al. | Colchicine-Induced Myopathy in a Tacrolimus-Treated Renal Transplant Recipient: Case Report and Literature Review. | Am J Ther | pmid:24732905 | |
| Lythgoe M and Abraham S | Tacrolimus: an effective treatment in refractory psoriatic arthritis following biologic failure. | Clin. Exp. Rheumatol. | pmid:26211753 | |
| Leon L et al. | Successfull Simultaneous Pancreas Kidney transplantation in a patient with Congenital Partial Lipodystrophy. | Nefrologia | pmid:27006329 |