| MeSH term | MeSH ID | Detail |
|---|---|---|
| Scorpion Stings | D065008 | 1 associated lipids |
| Drug-Related Side Effects and Adverse Reactions | D064420 | 3 associated lipids |
| Retrognathia | D063173 | 1 associated lipids |
| End Stage Liver Disease | D058625 | 1 associated lipids |
| Candidiasis, Invasive | D058365 | 2 associated lipids |
| Acute Kidney Injury | D058186 | 34 associated lipids |
| Thrombotic Microangiopathies | D057049 | 1 associated lipids |
| Central Serous Chorioretinopathy | D056833 | 1 associated lipids |
| Leukoencephalopathies | D056784 | 3 associated lipids |
| Netherton Syndrome | D056770 | 1 associated lipids |
| Latent Tuberculosis | D055985 | 1 associated lipids |
| Invasive Pulmonary Aspergillosis | D055744 | 1 associated lipids |
| Keratosis, Actinic | D055623 | 3 associated lipids |
| Multiple Pulmonary Nodules | D055613 | 2 associated lipids |
| Pancreatitis, Graft | D055589 | 1 associated lipids |
| Failed Back Surgery Syndrome | D055111 | 3 associated lipids |
| Primary Graft Dysfunction | D055031 | 1 associated lipids |
| Idiopathic Interstitial Pneumonias | D054988 | 1 associated lipids |
| Dendritic Cell Sarcoma, Interdigitating | D054739 | 1 associated lipids |
| Precursor Cell Lymphoblastic Leukemia-Lymphoma | D054198 | 10 associated lipids |
| Posterior Leukoencephalopathy Syndrome | D054038 | 1 associated lipids |
| Dysuria | D053159 | 1 associated lipids |
| Nocturia | D053158 | 1 associated lipids |
| Delayed Graft Function | D051799 | 2 associated lipids |
| Renal Insufficiency | D051437 | 8 associated lipids |
| Lymphohistiocytosis, Hemophagocytic | D051359 | 1 associated lipids |
| Granulomatosis, Orofacial | D051261 | 2 associated lipids |
| Atherosclerosis | D050197 | 85 associated lipids |
| Dyslipidemias | D050171 | 7 associated lipids |
| Diabetes Complications | D048909 | 4 associated lipids |
| Hepatic Insufficiency | D048550 | 1 associated lipids |
| Colitis, Collagenous | D046729 | 1 associated lipids |
| Protoporphyria, Erythropoietic | D046351 | 1 associated lipids |
| Coproporphyria, Hereditary | D046349 | 1 associated lipids |
| Ileus | D045823 | 3 associated lipids |
| Intestinal Volvulus | D045822 | 1 associated lipids |
| Cholecystolithiasis | D041761 | 2 associated lipids |
| Mastocytosis, Cutaneous | D034701 | 1 associated lipids |
| Hypoalbuminemia | D034141 | 1 associated lipids |
| Hyperuricemia | D033461 | 4 associated lipids |
| Papillomavirus Infections | D030361 | 4 associated lipids |
| Denys-Drash Syndrome | D030321 | 1 associated lipids |
| Pulmonary Disease, Chronic Obstructive | D029424 | 16 associated lipids |
| Polyomavirus Infections | D027601 | 1 associated lipids |
| Coronary Stenosis | D023921 | 6 associated lipids |
| Lacerations | D022125 | 1 associated lipids |
| Brachial Plexus Neuritis | D020968 | 2 associated lipids |
| Neuroaspergillosis | D020953 | 2 associated lipids |
| Hypoxia-Ischemia, Brain | D020925 | 22 associated lipids |
| Central Nervous System Viral Diseases | D020805 | 1 associated lipids |
| Intracranial Thrombosis | D020767 | 2 associated lipids |
| Parkinsonian Disorders | D020734 | 20 associated lipids |
| Nervous System Autoimmune Disease, Experimental | D020721 | 3 associated lipids |
| Stroke | D020521 | 32 associated lipids |
| Brain Infarction | D020520 | 17 associated lipids |
| Peroneal Neuropathies | D020427 | 1 associated lipids |
| Sciatic Neuropathy | D020426 | 13 associated lipids |
| Osteoarthritis, Knee | D020370 | 13 associated lipids |
| Paraneoplastic Syndromes, Nervous System | D020361 | 1 associated lipids |
| Hypertensive Encephalopathy | D020343 | 1 associated lipids |
| Migraine with Aura | D020325 | 1 associated lipids |
| Autoimmune Diseases of the Nervous System | D020274 | 1 associated lipids |
| Neurotoxicity Syndromes | D020258 | 34 associated lipids |
| Ventricular Remodeling | D020257 | 28 associated lipids |
| Infarction, Middle Cerebral Artery | D020244 | 35 associated lipids |
| Optic Nerve Injuries | D020221 | 4 associated lipids |
| Facial Nerve Injuries | D020220 | 1 associated lipids |
| Trauma, Nervous System | D020196 | 2 associated lipids |
| Nocturnal Myoclonus Syndrome | D020189 | 1 associated lipids |
| Sleep Apnea, Central | D020182 | 1 associated lipids |
| Citrullinemia | D020159 | 1 associated lipids |
| Hepatopulmonary Syndrome | D020065 | 1 associated lipids |
| Epstein-Barr Virus Infections | D020031 | 3 associated lipids |
| Genetic Predisposition to Disease | D020022 | 24 associated lipids |
| Miller Fisher Syndrome | D019846 | 1 associated lipids |
| Hepatitis C, Chronic | D019698 | 12 associated lipids |
| Hepatitis B, Chronic | D019694 | 4 associated lipids |
| Hepatitis, Autoimmune | D019693 | 1 associated lipids |
| Neurodegenerative Diseases | D019636 | 32 associated lipids |
| Intracranial Hypertension | D019586 | 4 associated lipids |
| Dermatitis, Perioral | D019557 | 4 associated lipids |
| Pouchitis | D019449 | 3 associated lipids |
| Endotoxemia | D019446 | 27 associated lipids |
| Oral Ulcer | D019226 | 1 associated lipids |
| Gingival Overgrowth | D019214 | 7 associated lipids |
| Fasciitis, Necrotizing | D019115 | 1 associated lipids |
| Postoperative Hemorrhage | D019106 | 7 associated lipids |
| Multiple Endocrine Neoplasia Type 2a | D018813 | 1 associated lipids |
| Anemia, Iron-Deficiency | D018798 | 6 associated lipids |
| Encephalitis, Viral | D018792 | 3 associated lipids |
| Hypoplastic Left Heart Syndrome | D018636 | 1 associated lipids |
| Cryptogenic Organizing Pneumonia | D018549 | 3 associated lipids |
| Ventricular Dysfunction, Left | D018487 | 33 associated lipids |
| Lichen Sclerosus et Atrophicus | D018459 | 2 associated lipids |
| Vasculitis, Leukocytoclastic, Cutaneous | D018366 | 5 associated lipids |
| Hutchinson's Melanotic Freckle | D018327 | 2 associated lipids |
| Angiofibroma | D018322 | 2 associated lipids |
| Cervical Intraepithelial Neoplasia | D018290 | 1 associated lipids |
| Seminoma | D018239 | 2 associated lipids |
| Smooth Muscle Tumor | D018235 | 1 associated lipids |
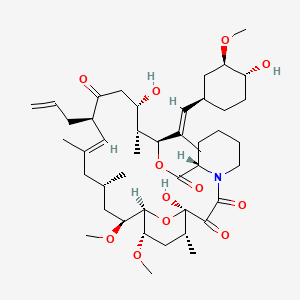
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- Am. J. Physiol. Renal Physiol. (1)
- Drug Metab. Dispos. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Yang J et al. | Zinc finger protein A20 protects rats against chronic liver allograft dysfunction. | 2012 | World J. Gastroenterol. | pmid:22826618 |
| Chen ZS et al. | Early steroid withdrawal after liver transplantation for hepatocellular carcinoma. | 2007 | World J. Gastroenterol. | pmid:17876900 |
| Zhou J et al. | Conversion to sirolimus immunosuppression in liver transplantation recipients with hepatocellular carcinoma: Report of an initial experience. | 2006 | World J. Gastroenterol. | pmid:16718799 |
| Li DW et al. | Risk factors for new onset diabetes mellitus after liver transplantation: A meta-analysis. | 2015 | World J. Gastroenterol. | pmid:26034369 |
| Guo YW et al. | Successful treatment of ileal ulcers caused by immunosuppressants in two organ transplant recipients. | 2016 | World J. Gastroenterol. | pmid:27350740 |
| Kang YZ et al. | Autoimmune hepatitis-primary biliary cirrhosis concurrent with biliary stricture after liver transplantation. | 2015 | World J. Gastroenterol. | pmid:25717264 |
| Schumacher G et al. | Sirolimus inhibits growth of human hepatoma cells alone or combined with tacrolimus, while tacrolimus promotes cell growth. | 2005 | World J. Gastroenterol. | pmid:15770715 |
| Hilgard P et al. | Cyclosporine versus tacrolimus in patients with HCV infection after liver transplantation: effects on virus replication and recurrent hepatitis. | 2006 | World J. Gastroenterol. | pmid:16521181 |
| Eshraghian A et al. | Post-transplant lymphoproliferative disorder after liver transplantation: Incidence, long-term survival and impact of serum tacrolimus level. | 2017 | World J. Gastroenterol. | pmid:28275302 |
| Jiang JW et al. | Optimal immunosuppressor induces stable gut microbiota after liver transplantation. | 2018 | World J. Gastroenterol. | pmid:30228781 |
| Liu C et al. | Cyclosporine A, FK-506, 40-0-[2-hydroxyethyl]rapamycin and mycophenolate mofetil inhibit proliferation of human intrahepatic biliary epithelial cells in vitro. | 2005 | World J. Gastroenterol. | pmid:16437685 |
| Lan X et al. | Efficacy of immunosuppression monotherapy after liver transplantation: a meta-analysis. | 2014 | World J. Gastroenterol. | pmid:25232269 |
| Del Bello A et al. | High tacrolimus intra-patient variability is associated with graft rejection, and donor-specific antibodies occurrence after liver transplantation. | 2018 | World J. Gastroenterol. | pmid:29713132 |
| Akamatsu N et al. | Late-onset acute rejection after living donor liver transplantation. | 2006 | World J. Gastroenterol. | pmid:17075982 |
| Larsen FS et al. | Low-dose tacrolimus ameliorates liver inflammation and fibrosis in steroid refractory autoimmune hepatitis. | 2007 | World J. Gastroenterol. | pmid:17589903 |
| Wietzke-Braun P et al. | Initial steroid-free immunosuppression after liver transplantation in recipients with hepatitis C virus related cirrhosis. | 2004 | World J. Gastroenterol. | pmid:15259068 |
| Higashi H et al. | First successful perinatal management of pregnancy after ABO-incompatible liver transplantation. | 2017 | World J. Gastroenterol. | pmid:28210092 |
| Shao ZY et al. | Prophylaxis of chronic kidney disease after liver transplantation--experience from west China. | 2012 | World J. Gastroenterol. | pmid:22408361 |
| Indriolo A and Ravelli P | Clinical management of inflammatory bowel disease in the organ recipient. | 2014 | World J. Gastroenterol. | pmid:24707135 |
| Shen T et al. | Reversible sinusoidal obstruction syndrome associated with tacrolimus following liver transplantation. | 2015 | World J. Gastroenterol. | pmid:26034381 |