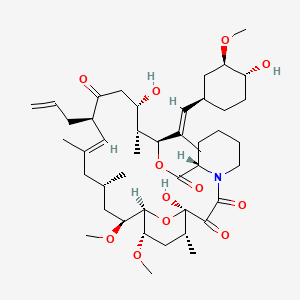
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- Am. J. Physiol. Renal Physiol. (1)
- Drug Metab. Dispos. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Lehmann R et al. | Successful simultaneous islet-kidney transplantation using a steroid-free immunosuppression: two-year follow-up. | 2004 | Am. J. Transplant. | pmid:15196070 |
| Knoop C et al. | Tacrolimus pharmacokinetics and dose monitoring after lung transplantation for cystic fibrosis and other conditions. | 2005 | Am. J. Transplant. | pmid:15888057 |
| Kim EJ et al. | Costimulation blockade alters germinal center responses and prevents antibody-mediated rejection. | 2014 | Am. J. Transplant. | pmid:24354871 |
| Kandaswamy R et al. | A prospective randomized trial of steroid-free maintenance regimens in kidney transplant recipients--an interim analysis. | 2005 | Am. J. Transplant. | pmid:15888064 |
| Cavadas PC et al. | Bilateral trans-humeral arm transplantation: result at 2 years. | 2011 | Am. J. Transplant. | pmid:21521475 |
| Xu H et al. | The allo- and viral-specific immunosuppressive effect of belatacept, but not tacrolimus, attenuates with progressive T cell maturation. | 2014 | Am. J. Transplant. | pmid:24472192 |
| Qazi Y et al. | Efficacy and Safety of Everolimus Plus Low-Dose Tacrolimus Versus Mycophenolate Mofetil Plus Standard-Dose Tacrolimus in De Novo Renal Transplant Recipients: 12-Month Data. | 2017 | Am. J. Transplant. | pmid:27775865 |
| Coghill AE et al. | Immunosuppressive Medications and Squamous Cell Skin Carcinoma: Nested Case-Control Study Within the Skin Cancer after Organ Transplant (SCOT) Cohort. | 2016 | Am. J. Transplant. | pmid:26824445 |
| Zafrani L et al. | Incidence, risk factors and clinical consequences of neutropenia following kidney transplantation: a retrospective study. | 2009 | Am. J. Transplant. | pmid:19538494 |
| Touzot M et al. | Renal transplantation in HIV-infected patients: the Paris experience. | 2010 | Am. J. Transplant. | pmid:20840478 |
| Krämer BK et al. | Tacrolimus once daily (ADVAGRAF) versus twice daily (PROGRAF) in de novo renal transplantation: a randomized phase III study. | 2010 | Am. J. Transplant. | pmid:20840480 |
| TruneÄka P et al. | Once-daily prolonged-release tacrolimus (ADVAGRAF) versus twice-daily tacrolimus (PROGRAF) in liver transplantation. | 2010 | Am. J. Transplant. | pmid:20840481 |
| Mehra MR et al. | Immunosuppression in cardiac transplantation: science, common sense and the heart of the matter. | 2006 | Am. J. Transplant. | pmid:16686745 |
| Grimm M et al. | Superior prevention of acute rejection by tacrolimus vs. cyclosporine in heart transplant recipients--a large European trial. | 2006 | Am. J. Transplant. | pmid:16686762 |
| Budde K et al. | Novel once-daily extended-release tacrolimus (LCPT) versus twice-daily tacrolimus in de novo kidney transplants: one-year results of Phase III, double-blind, randomized trial. | 2014 | Am. J. Transplant. | pmid:25278376 |
| O'Grady JG et al. | Randomized controlled trial of tacrolimus versus microemulsified cyclosporin (TMC) in liver transplantation: poststudy surveillance to 3 years. | 2007 | Am. J. Transplant. | pmid:17109723 |
| Böhmig GA et al. | Immunoadsorption in severe C4d-positive acute kidney allograft rejection: a randomized controlled trial. | 2007 | Am. J. Transplant. | pmid:17109725 |
| Budde K et al. | Sotrastaurin, a novel small molecule inhibiting protein kinase C: first clinical results in renal-transplant recipients. | 2010 | Am. J. Transplant. | pmid:20121745 |
| Al-Massarani G et al. | Impact of immunosuppressive treatment on endothelial biomarkers after kidney transplantation. | 2008 | Am. J. Transplant. | pmid:18925903 |
| Bouamar R et al. | Tacrolimus predose concentrations do not predict the risk of acute rejection after renal transplantation: a pooled analysis from three randomized-controlled clinical trials(†). | 2013 | Am. J. Transplant. | pmid:23480233 |
| Busque S et al. | The PROMISE study: a phase 2b multicenter study of voclosporin (ISA247) versus tacrolimus in de novo kidney transplantation. | 2011 | Am. J. Transplant. | pmid:21943027 |
| Hamdy AF et al. | Comparison of sirolimus with low-dose tacrolimus versus sirolimus-based calcineurin inhibitor-free regimen in live donor renal transplantation. | 2005 | Am. J. Transplant. | pmid:16162204 |
| Kaufman DB et al. | Alemtuzumab induction and prednisone-free maintenance immunotherapy in kidney transplantation: comparison with basiliximab induction--long-term results. | 2005 | Am. J. Transplant. | pmid:16162205 |
| Naesens M et al. | Tacrolimus exposure and evolution of renal allograft histology in the first year after transplantation. | 2007 | Am. J. Transplant. | pmid:17608835 |
| Schwarz A et al. | Polyoma virus nephropathy in native kidneys after lung transplantation. | 2005 | Am. J. Transplant. | pmid:16162212 |
| Shemesh E et al. | The Medication Level Variability Index (MLVI) Predicts Poor Liver Transplant Outcomes: A Prospective Multi-Site Study. | 2017 | Am. J. Transplant. | pmid:28321975 |
| Troppmann C et al. | Impact of portal venous pancreas graft drainage on kidney graft outcome in simultaneous pancreas-kidney recipients reported to UNOS. | 2004 | Am. J. Transplant. | pmid:15023146 |
| Muthusamy AS et al. | Alemtuzumab induction and steroid-free maintenance immunosuppression in pancreas transplantation. | 2008 | Am. J. Transplant. | pmid:18828772 |
| Van Laecke S et al. | Posttransplantation hypomagnesemia and its relation with immunosuppression as predictors of new-onset diabetes after transplantation. | 2009 | Am. J. Transplant. | pmid:19624560 |
| Pirenne J et al. | Tolerance of liver transplant patients to strenuous physical activity in high-altitude. | 2004 | Am. J. Transplant. | pmid:15023147 |
| Heisel O et al. | New onset diabetes mellitus in patients receiving calcineurin inhibitors: a systematic review and meta-analysis. | 2004 | Am. J. Transplant. | pmid:15023151 |
| Hardinger KL et al. | Pharmacokinetics of tacrolimus in kidney transplant recipients: twice daily versus once daily dosing. | 2004 | Am. J. Transplant. | pmid:15023155 |
| Suwelack B et al. | Withdrawal of cyclosporine or tacrolimus after addition of mycophenolate mofetil in patients with chronic allograft nephropathy. | 2004 | Am. J. Transplant. | pmid:15023160 |
| Diaz-Siso JR et al. | Initial experience of dual maintenance immunosuppression with steroid withdrawal in vascular composite tissue allotransplantation. | 2015 | Am. J. Transplant. | pmid:25777324 |
| Rodriguez-Rodriguez AE et al. | The higher diabetogenic risk of tacrolimus depends on pre-existing insulin resistance. A study in obese and lean Zucker rats. | 2013 | Am. J. Transplant. | pmid:23651473 |
| Klintmalm GB et al. | Belatacept-based immunosuppression in de novo liver transplant recipients: 1-year experience from a phase II randomized study. | 2014 | Am. J. Transplant. | pmid:25041339 |
| TruneÄŒka P et al. | Renal Function in De Novo Liver Transplant Recipients Receiving Different Prolonged-Release Tacrolimus Regimens-The DIAMOND Study. | 2015 | Am. J. Transplant. | pmid:25707487 |
| Oetting WS et al. | Genomewide Association Study of Tacrolimus Concentrations in African American Kidney Transplant Recipients Identifies Multiple CYP3A5 Alleles. | 2016 | Am. J. Transplant. | pmid:26485092 |
| Badri P et al. | Pharmacokinetics and dose recommendations for cyclosporine and tacrolimus when coadministered with ABT-450, ombitasvir, and dasabuvir. | 2015 | Am. J. Transplant. | pmid:25708713 |
| Larson TS et al. | Complete avoidance of calcineurin inhibitors in renal transplantation: a randomized trial comparing sirolimus and tacrolimus. | 2006 | Am. J. Transplant. | pmid:16468960 |
| Vitko S et al. | Tacrolimus combined with two different dosages of sirolimus in kidney transplantation: results of a multicenter study. | 2006 | Am. J. Transplant. | pmid:16468962 |
| Luan FL et al. | Comparative risk of impaired glucose metabolism associated with cyclosporine versus tacrolimus in the late posttransplant period. | 2008 | Am. J. Transplant. | pmid:18786231 |
| Woywodt A et al. | Different preparations of tacrolimus and medication errors. | 2008 | Am. J. Transplant. | pmid:18786238 |
| Servais A et al. | Interstitial fibrosis evolution on early sequential screening renal allograft biopsies using quantitative image analysis. | 2011 | Am. J. Transplant. | pmid:21672152 |
| Bourdeaux C et al. | Living-related versus deceased donor pediatric liver transplantation: a multivariate analysis of technical and immunological complications in 235 recipients. | 2007 | Am. J. Transplant. | pmid:17173657 |
| Ryan CM and Swanson DP | clinical research, innovative practice and IRB review: identifying and respecting boundaries. | 2007 | Am. J. Transplant. | pmid:17331113 |
| Rostaing L et al. | Alefacept combined with tacrolimus, mycophenolate mofetil and steroids in de novo kidney transplantation: a randomized controlled trial. | 2013 | Am. J. Transplant. | pmid:23730730 |
| Pradhan M et al. | Decline in renal function following thoracic organ transplantation in children. | 2002 | Am. J. Transplant. | pmid:12201367 |
| Ciancio G et al. | Advantage of rapamycin over mycophenolate mofetil when used with tacrolimus for simultaneous pancreas kidney transplants: randomized, single-center trial at 10 years. | 2012 | Am. J. Transplant. | pmid:22946986 |
| Jacobson PA et al. | Lower calcineurin inhibitor doses in older compared to younger kidney transplant recipients yield similar troughs. | 2012 | Am. J. Transplant. | pmid:22947444 |