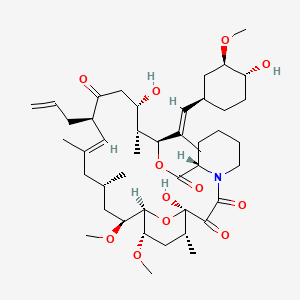
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- Am. J. Physiol. Renal Physiol. (1)
- Drug Metab. Dispos. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Franke EK and Luban J | Inhibition of HIV-1 replication by cyclosporine A or related compounds correlates with the ability to disrupt the Gag-cyclophilin A interaction. | 1996 | Virology | pmid:8806510 |
| Mahalingam R et al. | Simian varicella virus reactivation in cynomolgus monkeys. | 2007 | Virology | pmid:17651776 |
| Goldfeld AE et al. | Cyclosporin A and FK506 block induction of the Epstein-Barr virus lytic cycle by anti-immunoglobulin. | 1995 | Virology | pmid:7538254 |
| Juvvadi PR et al. | Calcineurin in fungal virulence and drug resistance: Prospects for harnessing targeted inhibition of calcineurin for an antifungal therapeutic approach. | 2017 | Virulence | pmid:27325145 |
| Carbajo-Lozoya J et al. | Human coronavirus NL63 replication is cyclophilin A-dependent and inhibited by non-immunosuppressive cyclosporine A-derivatives including Alisporivir. | 2014 | Virus Res. | pmid:24566223 |
| Carbajo-Lozoya J et al. | Replication of human coronaviruses SARS-CoV, HCoV-NL63 and HCoV-229E is inhibited by the drug FK506. | 2012 | Virus Res. | pmid:22349148 |
| Kass L et al. | Inhibition of the calcineurin-like protein phosphatase activity in Limulus ventral eye photoreceptor cells alters the characteristics of the spontaneous quantal bumps and the light-mediated inward currents, and enhances arrestin phosphorylation. | 1998 Nov-Dec | Vis. Neurosci. | pmid:9839968 |
| TruneÄka P | [Immunosuppression after liver transplant, now and in future]. | 2013 | Vnitr Lek | pmid:24007221 |
| Bakardzhiev I et al. | Unilateral unique Lupus tumidus: pathogenetic mystery and diagnostic problem. | 2016 | Wien Med Wochenschr | pmid:26762262 |
| Durrant-Finn U et al. | [Pruritus and dryness of the skin in chronic kidney insufficiency and dialysis patients - a review]. | 2009 | Wien Med Wochenschr | pmid:19652938 |
| Schwarz C et al. | Rescue therapy with tacrolimus and mycophenolate mofetil does not prevent deterioration of graft function in C4d-positive chronic allograft nephropathy. | 2006 | Wien. Klin. Wochenschr. | pmid:16865644 |
| Sperr WR et al. | [Effector cells in allergy: biological principles and new pharmacologic concepts]. | 1993 | Wien. Klin. Wochenschr. | pmid:7508662 |
| Haas M et al. | Hypothyroidism as a cause of tacrolimus intoxication and acute renal failure: a case report. | 2000 | Wien. Klin. Wochenschr. | pmid:11144010 |
| Zong YP et al. | Effects of CYP3A5 polymorphisms on tacrolimus pharmacokinetics in pediatric kidney transplantation: a systematic review and meta-analysis of observational studies. | 2017 | World J Pediatr | pmid:28540692 |
| Yang EM et al. | Tacrolimus for children with refractory nephrotic syndrome: a one-year prospective, multicenter, and open-label study of Tacrobell®, a generic formula. | 2016 | World J Pediatr | pmid:26684309 |
| Kallash M and Aviles D | Efficacy of tacrolimus in the treatment of children with focal segmental glomerulosclerosis. | 2014 | World J Pediatr | pmid:24801235 |
| Schlosser K et al. | Surgical treatment of tertiary hyperparathyroidism: the choice of procedure matters! | 2007 | World J Surg | pmid:17665243 |
| Platz KP et al. | Management of acute steroid-resistant rejection after liver transplantation. | 1996 | World J Surg | pmid:8798364 |
| Sutherland DE et al. | Pancreas transplantation for treatment of diabetes mellitus. | 2001 | World J Surg | pmid:11344403 |
| Kato T et al. | Intestinal and multivisceral transplantation. | 2002 | World J Surg | pmid:11865353 |
| Motoyama K et al. | Pretransplant intrathymic inoculation of donor antigen combined with FK506 treatment: prolongation of survival of cardiac, but not renal, allografts in rats. | 1995 Mar-Apr | World J Surg | pmid:7538717 |
| Ramakant P and Agarwal G | Surgical treatment of tertiary hyperparathyroidism: the choice of procedure matters: surgical management of tertiary hyperparathyroidism: an enigma. | 2008 | World J Surg | pmid:18404286 |
| Montenegro F et al. | Surgical treatment of tertiary hyperparathyroidism: the choice of procedure matters! | 2008 | World J Surg | pmid:18204944 |
| Jordan ML et al. | The use of tacrolimus in renal transplantation. | 1996 | World J Urol | pmid:8873438 |
| Yang J et al. | Zinc finger protein A20 protects rats against chronic liver allograft dysfunction. | 2012 | World J. Gastroenterol. | pmid:22826618 |
| Zhou J et al. | Conversion to sirolimus immunosuppression in liver transplantation recipients with hepatocellular carcinoma: Report of an initial experience. | 2006 | World J. Gastroenterol. | pmid:16718799 |
| Song JL et al. | Minimizing tacrolimus decreases the risk of new-onset diabetes mellitus after liver transplantation. | 2016 | World J. Gastroenterol. | pmid:26877618 |
| Filipec Kanizaj T and Mijic M | Inflammatory bowel disease in liver transplanted patients. | 2017 | World J. Gastroenterol. | pmid:28566881 |
| Provenzani A et al. | Pharmacogenetic considerations for optimizing tacrolimus dosing in liver and kidney transplant patients. | 2013 | World J. Gastroenterol. | pmid:24409044 |
| Guo YW et al. | Successful treatment of ileal ulcers caused by immunosuppressants in two organ transplant recipients. | 2016 | World J. Gastroenterol. | pmid:27350740 |
| Kang YZ et al. | Autoimmune hepatitis-primary biliary cirrhosis concurrent with biliary stricture after liver transplantation. | 2015 | World J. Gastroenterol. | pmid:25717264 |
| Liu F et al. | Tacrolimus dosage requirements in living donor liver transplant recipients with small-for-size grafts. | 2009 | World J. Gastroenterol. | pmid:19701975 |
| Schott E et al. | Development of ulcerative colitis in a patient with multiple sclerosis following treatment with interferon beta 1a. | 2007 | World J. Gastroenterol. | pmid:17659718 |
| Schumacher G et al. | Sirolimus inhibits growth of human hepatoma cells alone or combined with tacrolimus, while tacrolimus promotes cell growth. | 2005 | World J. Gastroenterol. | pmid:15770715 |
| Jia JJ et al. | ''Minimizing tacrolimus'' strategy and long-term survival after liver transplantation. | 2014 | World J. Gastroenterol. | pmid:25170223 |
| Hao JC et al. | Effect of low-dose tacrolimus with mycophenolate mofetil on renal function following liver transplantation. | 2014 | World J. Gastroenterol. | pmid:25170222 |
| Takeichi T et al. | Effect of ONO-4057 and tacrolimus on ischemia-reperfusion injury of the liver. | 2009 | World J. Gastroenterol. | pmid:19960569 |
| Eshraghian A et al. | Post-transplant lymphoproliferative disorder after liver transplantation: Incidence, long-term survival and impact of serum tacrolimus level. | 2017 | World J. Gastroenterol. | pmid:28275302 |
| Wu SY et al. | Comprehensive risk assessment for early neurologic complications after liver transplantation. | 2016 | World J. Gastroenterol. | pmid:27350733 |
| Liu C et al. | Cyclosporine A, FK-506, 40-0-[2-hydroxyethyl]rapamycin and mycophenolate mofetil inhibit proliferation of human intrahepatic biliary epithelial cells in vitro. | 2005 | World J. Gastroenterol. | pmid:16437685 |
| Kawakami K et al. | Effects of oral tacrolimus as a rapid induction therapy in ulcerative colitis. | 2015 | World J. Gastroenterol. | pmid:25684955 |
| Lan X et al. | Efficacy of immunosuppression monotherapy after liver transplantation: a meta-analysis. | 2014 | World J. Gastroenterol. | pmid:25232269 |
| Del Bello A et al. | High tacrolimus intra-patient variability is associated with graft rejection, and donor-specific antibodies occurrence after liver transplantation. | 2018 | World J. Gastroenterol. | pmid:29713132 |
| Meier J and Sturm A | Current treatment of ulcerative colitis. | 2011 | World J. Gastroenterol. | pmid:21912469 |
| Okan G et al. | Vanishing bile duct and Stevens-Johnson syndrome associated with ciprofloxacin treated with tacrolimus. | 2008 | World J. Gastroenterol. | pmid:18698687 |
| Akamatsu N et al. | Late-onset acute rejection after living donor liver transplantation. | 2006 | World J. Gastroenterol. | pmid:17075982 |
| Wietzke-Braun P et al. | Initial steroid-free immunosuppression after liver transplantation in recipients with hepatitis C virus related cirrhosis. | 2004 | World J. Gastroenterol. | pmid:15259068 |
| Higashi H et al. | First successful perinatal management of pregnancy after ABO-incompatible liver transplantation. | 2017 | World J. Gastroenterol. | pmid:28210092 |
| Shao ZY et al. | Prophylaxis of chronic kidney disease after liver transplantation--experience from west China. | 2012 | World J. Gastroenterol. | pmid:22408361 |
| Buchholz BM et al. | Role of colectomy in preventing recurrent primary sclerosing cholangitis in liver transplant recipients. | 2018 | World J. Gastroenterol. | pmid:30065563 |