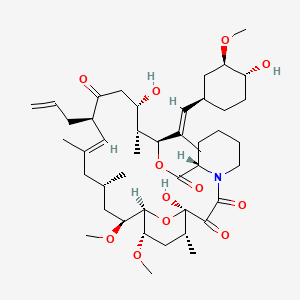
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Mehta RS et al. | Post-transplantation cyclophosphamide versus conventional graft-versus-host disease prophylaxis in mismatched unrelated donor haematopoietic cell transplantation. | 2016 | Br. J. Haematol. | pmid:26947769 |
| Kiyohara H et al. | Up-to-date medical treatment for ulcerative colitis. | 2016 | Nihon Shokakibyo Gakkai Zasshi | pmid:26947041 |
| Carcas-Sansuán AJ | Limited sampling strategies for once daily tacrolimus exposure monitoring. | 2016 | Eur. J. Clin. Pharmacol. | pmid:26939899 |
| Iguchi A et al. | Graft-versus-host disease (GVHD) prophylaxis by using methotrexate decreases pre-engraftment syndrome and severe acute GVHD, and accelerates engraftment after cord blood transplantation. | 2016 | Pediatr Transplant | pmid:26526424 |
| Fukuta T et al. | Non-invasive evaluation of neuroprotective drug candidates for cerebral infarction by PET imaging of mitochondrial complex-I activity. | 2016 | Sci Rep | pmid:27440054 |
| Dugast E et al. | Failure of Calcineurin Inhibitor (Tacrolimus) Weaning Randomized Trial in Long-Term Stable Kidney Transplant Recipients. | 2016 | Am. J. Transplant. | pmid:27367750 |
| Kolb M et al. | Risk Factors for Subtherapeutic Tacrolimus Levels after Conversion from Continuous Intravenous Infusion to Oral in Children after Allogeneic Hematopoietic Cell Transplantation. | 2016 | Biol. Blood Marrow Transplant. | pmid:26880117 |
| Arreola-Guerra JM et al. | Tacrolimus Trough Levels as a Risk Factor for Acute Rejection in Renal Transplant Patients. | 2016 | Ann. Transplant. | pmid:26879833 |
| Žilinská Z et al. | Impact of Trough Levels of Tacrolimus on Kidney Function and Graft Survival in Short and Longer Periods After Renal Transplantation. | 2016 | Transplant. Proc. | pmid:27788794 |
| Dharnidharka VR et al. | Differential risks for adverse outcomes 3 years after kidney transplantation based on initial immunosuppression regimen: a national study. | 2016 | Transpl. Int. | pmid:27564782 |
| Rostaing L et al. | Successful Transplantation in ABO- and HLA-Incompatible Living Kidney Transplant Patients: A Report on 12 Cases. | 2016 | Ther Apher Dial | pmid:27073167 |
| Pirojsakul K et al. | Management of sensitized pediatric patients prior to renal transplantation. | 2016 | Pediatr. Nephrol. | pmid:26801944 |
| Guo YW et al. | Successful treatment of ileal ulcers caused by immunosuppressants in two organ transplant recipients. | 2016 | World J. Gastroenterol. | pmid:27350740 |
| Nekkanti V et al. | Design, Characterization, and In Vivo Pharmacokinetics of Tacrolimus Proliposomes. | 2016 | AAPS PharmSciTech | pmid:26729532 |
| Armand P et al. | The addition of sirolimus to the graft-versus-host disease prophylaxis regimen in reduced intensity allogeneic stem cell transplantation for lymphoma: a multicentre randomized trial. | 2016 | Br. J. Haematol. | pmid:26729448 |
| Badr R et al. | Assessment of global ischemic/reperfusion and Tacrolimus administration on CA1 region of hippocampus: gene expression profiles of BAX and BCL2 genes. | 2016 | Bratisl Lek Listy | pmid:27546370 |
| Hanaoka K et al. | A chronic renal rejection model with a fully MHC-mismatched rat strain combination under immunosuppressive therapy. | 2016 | Transpl. Immunol. | pmid:27545900 |
| Matsa E et al. | Transcriptome Profiling of Patient-Specific Human iPSC-Cardiomyocytes Predicts Individual Drug Safety and Efficacy Responses In Vitro. | 2016 | Cell Stem Cell | pmid:27545504 |
| Thao le Q et al. | Pharmaceutical potential of tacrolimus-loaded albumin nanoparticles having targetability to rheumatoid arthritis tissues. | 2016 | Int J Pharm | pmid:26657273 |
| Mokuda S and Oiwa H | Successful treatment of FKBP51-expressed multicentric reticulohistiocytosis using combination therapy with low-dose denosumab and tacrolimus. | 2016 | Scand. J. Rheumatol. | pmid:26652057 |
| Albeiroti S et al. | Evaluation of 2 Batched Pretreatment Systems for the Measurement of Whole Blood Tacrolimus on the ARCHITECT Immunoassay Analyzer. | 2016 | Lab Med | pmid:27474776 |
| Yu H et al. | Risk factors for new-onset diabetes mellitus after living donor kidney transplantation in Korea - a retrospective single center study. | 2016 | BMC Nephrol | pmid:27473469 |
| Filler G et al. | Minimum mycophenolic acid levels are associated with donor-specific antibody formation. | 2016 | Pediatr Transplant | pmid:26589470 |
| Scalea JR et al. | Tacrolimus for the prevention and treatment of rejection of solid organ transplants. | 2016 | Expert Rev Clin Immunol | pmid:26588770 |
| Sakai R et al. | A comparison of tacrolimus and cyclosporine combined with methotrexate for graft-versus-host disease prophylaxis, stratified by stem cell source: a retrospective nationwide survey. | 2016 | Int. J. Hematol. | pmid:26800676 |
| Pouché L et al. | New challenges and promises in solid organ transplantation pharmacogenetics: the genetic variability of proteins involved in the pharmacodynamics of immunosuppressive drugs. | 2016 | Pharmacogenomics | pmid:26799749 |
| Wu SY et al. | Comprehensive risk assessment for early neurologic complications after liver transplantation. | 2016 | World J. Gastroenterol. | pmid:27350733 |
| Constantinescu AA et al. | Differential influence of tacrolimus and sirolimus on mitochondrial-dependent signaling for apoptosis in pancreatic cells. | 2016 | Mol. Cell. Biochem. | pmid:27344165 |
| Shao K et al. | Different Effects of Tacrolimus on Innate and Adaptive Immune Cells in the Allograft Transplantation. | 2016 | Scand. J. Immunol. | pmid:26524694 |
| Cena T et al. | De novo noncutaneous malignancies after kidney transplantation are associated with an increased risk of graft failure: results from a time-dependent analysis on 672 patients. | 2016 | Transpl. Int. | pmid:27343849 |
| Binkhathlan Z et al. | Reutilization of Tacrolimus Extracted from Expired Prograf® Capsules: Physical, Chemical, and Pharmacological Assessment. | 2016 | AAPS PharmSciTech | pmid:26729529 |
| Pizzo HP et al. | Sirolimus and tacrolimus coefficient of variation is associated with rejection, donor-specific antibodies, and nonadherence. | 2016 | Pediatr. Nephrol. | pmid:27286686 |
| Fernández de Castillo Torras L et al. | Treatment with ulipristal acetate (Esmya(®)) and plasma levels of tacrolimus: a case report. | 2016 | Eur. J. Obstet. Gynecol. Reprod. Biol. | pmid:27282803 |
| Youssef M et al. | Asymptomatic papulonodular lesions in zosteriform distribution in an immunocompromised patient. | 2016 | Int. J. Dermatol. | pmid:26463835 |
| Ferjani H et al. | The evaluate and compare the effects of the Tacrolimus and Sirolimus on the intestinal system using an intestinal cell culture model. | 2016 | Toxicol. Mech. Methods | pmid:26460985 |
| Sasaki T et al. | Characteristic features of tacrolimus-induced lung disease in rheumatoid arthritis patients. | 2016 | Clin. Rheumatol. | pmid:25644583 |
| Nerattini F et al. | II. Dissociation free energies in drug-receptor systems via nonequilibrium alchemical simulations: application to the FK506-related immunophilin ligands. | 2016 | Phys Chem Chem Phys | pmid:27193181 |
| O'Regan JA et al. | Tacrolimus trough-level variability predicts long-term allograft survival following kidney transplantation. | 2016 | J. Nephrol. | pmid:26374111 |
| Seok J et al. | Recalcitrant steroid-induced rosacea successfully treated with 0.03% tacrolimus and 595-nm pulsed dye laser. | 2016 | Eur J Dermatol | pmid:27193042 |
| Caillard S et al. | Advagraf(®) , a once-daily prolonged release tacrolimus formulation, in kidney transplantation: literature review and guidelines from a panel of experts. | 2016 | Transpl. Int. | pmid:26373896 |
| Reiner J et al. | After Intestinal Transplantation Kidney Function Is Impaired by Downregulation of Epithelial Ion Transporters in the Ileum. | 2016 | Transplant. Proc. | pmid:27109987 |
| Rao B et al. | Use of Everolimus After Multivisceral Transplantation: A Report of Two Cases. | 2016 | Transplant. Proc. | pmid:27109983 |
| Chang HK et al. | Ten-Year Experience With Bowel Transplantation at Seoul St. Mary's Hospital. | 2016 | Transplant. Proc. | pmid:27109981 |
| Kishida N et al. | Increased Incidence of Thrombotic Microangiopathy After ABO-Incompatible Living Donor Liver Transplantation. | 2016 | Ann. Transplant. | pmid:27956735 |
| Wang Y et al. | Preparation, characterization and in vivo evaluation of amorphous tacrolimus nanosuspensions produced using CO2-assisted in situ nanoamorphization method. | 2016 | Int J Pharm | pmid:27034003 |
| Jimbo H et al. | Telangiectatic lichen sclerosus on the cheek successfully treated with topical tacrolimus. | 2016 | Eur J Dermatol | pmid:27033557 |
| Shimizu K et al. | Specific delivery of an immunosuppressive drug to splenic B cells by antigen-modified liposomes and its antiallergic effect. | 2016 | J Drug Target | pmid:27030163 |
| Yan Y et al. | Robust Axonal Regeneration in a Mouse Vascularized Composite Allotransplant Model Undergoing Delayed Tissue Rejection. | 2016 | Hand (N Y) | pmid:28149214 |
| Carrillo-Ibarra S et al. | The Oxidative and Inflammatory State in Patients with Acute Renal Graft Dysfunction Treated with Tacrolimus. | 2016 | Oxid Med Cell Longev | pmid:27872679 |
| Thomusch O et al. | Rabbit-ATG or basiliximab induction for rapid steroid withdrawal after renal transplantation (Harmony): an open-label, multicentre, randomised controlled trial. | 2016 | Lancet | pmid:27871759 |