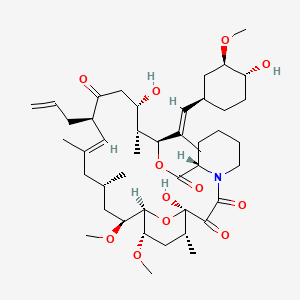
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- J. Pharmacol. Exp. Ther. (1)
- Am. J. Physiol. Renal Physiol. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Kanda J et al. | Effects of the calcineurin inhibitors cyclosporine and tacrolimus on bone metabolism in rats. | 2018 | Biomed. Res. | pmid:29899188 |
| Sikma MA et al. | Association of Whole Blood Tacrolimus Concentrations with Kidney Injury in Heart Transplantation Patients. | 2018 | Eur J Drug Metab Pharmacokinet | pmid:29236211 |
| Komura Y et al. | Economic assessment of actual prescription of drugs for treatment of atopic dermatitis: Differences between dermatology and pediatrics in large-scale receipt data. | 2018 | J. Dermatol. | pmid:29168213 |
| Cho EJ et al. | Performance of the Dimension TAC assay and comparison of multiple platforms for the measurement of tacrolimus. | 2018 | J. Clin. Lab. Anal. | pmid:29148096 |
| Sir G et al. | Antagonistic Effect of Oxytocin and Tacrolimus Combination on Adipose Tissue - Derived Mesenchymal Stem Cells: Antagonistic effect of oxytocin and tacrolimus. | 2018 | Biomed. Pharmacother. | pmid:29136956 |
| Wu MF et al. | Combination Therapy of Tacrolimus and Chinese Herb Medicated Bath in Children with Inverse Psoriasis. | 2018 | Chin J Integr Med | pmid:28914435 |
| Akamine Y et al. | A comparison of the effects of CYP3A5 polymorphism on tacrolimus blood concentrations measured by 4 immunoassay methods in renal transplant patients. | 2018 | J Clin Pharm Ther | pmid:28891077 |
| Ayala E et al. | Haploidentical transplantation as a promising therapy for relapsed hemophagocytic lymphohistiocytosis in an older adult patient. | 2018 | Hematol Oncol Stem Cell Ther | pmid:27352259 |
| Velioglu A et al. | Late Pulmonary Toxicity Associated With Everolimus in a Renal Transplant Patient and Review of the Literature. | 2018 | Exp Clin Transplant | pmid:27001620 |
| Hamano I et al. | Condyloma Acuminata of the Urethra in a Male Renal Transplant Recipient: A Case Report. | 2018 | Transplant. Proc. | pmid:30316397 |
| Choong CL et al. | Dose-Response Relationship Between Diltiazem and Tacrolimus and Its Safety in Renal Transplant Recipients. | 2018 | Transplant. Proc. | pmid:30316389 |
| Cheng CY et al. | Intervention of Online Percent Coefficient of Variation Reporting System Reduces the Variability of Tacrolimus Trough Concentration in Kidney Transplant Recipients. | 2018 | Transplant. Proc. | pmid:30316366 |
| Liu Y et al. | Delayed Initiation of Tacrolimus Is Safe and Effective in Renal Transplant Recipients With Delayed and Slow Graft Function. | 2018 | Transplant. Proc. | pmid:30316359 |
| Pflugrad H et al. | Longterm calcineurin inhibitor therapy and brain function in patients after liver transplantation. | 2018 | Liver Transpl. | pmid:29156491 |
| Loeschenberger B et al. | Calcineurin inhibitor-induced complement system activation via ERK1/2 signalling is inhibited by SOCS-3 in human renal tubule cells. | 2018 | Eur. J. Immunol. | pmid:29143318 |
| Tunnicliffe DJ et al. | Immunosuppressive treatment for proliferative lupus nephritis. | 2018 | Cochrane Database Syst Rev | pmid:29957821 |
| Sugahara S et al. | Integrin, alpha9 subunit blockade suppresses collagen-induced arthritis with minimal systemic immunomodulation. | 2018 | Eur. J. Pharmacol. | pmid:29932925 |
| Wen L et al. | Transient High Pressure in Pancreatic Ducts Promotes Inflammation and Alters Tight Junctions via Calcineurin Signaling in Mice. | 2018 | Gastroenterology | pmid:29928898 |
| Ohtsuki M et al. | Tacrolimus ointment for the treatment of adult and pediatric atopic dermatitis: Review on safety and benefits. | 2018 | J. Dermatol. | pmid:29927498 |
| Shimoda-Komatsu Y et al. | Chronological observation of surgically-treated granuloma faciale implies the necessity of circumspect management for perinasal nodular subset. | 2018 | J. Dermatol. | pmid:29905388 |
| Hou Y et al. | Management of hepatic vein occlusive disease after liver transplantation: A case report with literature review. | 2018 | Medicine (Baltimore) | pmid:29901618 |
| Özçakar ZB et al. | Transplantation within the era of anti-IL-1 therapy: case series of five patients with familial Mediterranean fever-related amyloidosis. | 2018 | Transpl. Int. | pmid:29957882 |
| Chao YH et al. | Tolerogenic β2-glycoprotein I DNA vaccine and FK506 as an adjuvant attenuates experimental obstetric antiphospholipid syndrome. | 2018 | PLoS ONE | pmid:29894515 |
| Lin G et al. | Evaluation of tacrolimus-related CYP3A5 genotyping in China: Results from the First External Quality Assessment Exercise. | 2018 | J. Clin. Lab. Anal. | pmid:29708622 |
| Luaces-RodrÃguez A et al. | Preclinical characterization and clinical evaluation of tacrolimus eye drops. | 2018 | Eur J Pharm Sci | pmid:29705214 |
| Castedal M et al. | Steroid-free immunosuppression with low-dose tacrolimus is safe and significantly reduces the incidence of new-onset diabetes mellitus following liver transplantation. | 2018 | Scand. J. Gastroenterol. | pmid:29688072 |
| Zhang Y and Zhang R | Recent advances in analytical methods for the therapeutic drug monitoring of immunosuppressive drugs. | 2018 | Drug Test Anal | pmid:28851030 |
| Niel O and Bastard P | Artificial intelligence improves estimation of tacrolimus area under the concentration over time curve in renal transplant recipients. | 2018 | Transpl. Int. | pmid:29687486 |
| Gmitterová K et al. | Tacrolimus-induced parkinsonism in a patient after liver transplantation - case report. | 2018 | BMC Neurol | pmid:29678162 |
| Liu HY et al. | Ribavirin-induced anaemia reduced tacrolimus level in a hepatitis C patient receiving haemodialysis. | 2018 | BMJ Case Rep | pmid:29669765 |
| Majeed A et al. | A 20-year experience with nocardiosis in solid organ transplant (SOT) recipients in the Southwestern United States: A single-center study. | 2018 | Transpl Infect Dis | pmid:29668074 |
| Mah A et al. | Graft loss attributed to possible transfusion-transmitted ehrlichiosis following cord blood stem cell transplant. | 2018 | Transpl Infect Dis | pmid:29668040 |
| Hong D et al. | [Atopic keratoconjunctivitis: One allergy may mask another. A clinical observation with two types of hypersensitivity reactions: IgE-mediated and non-IgE-mediated]. | 2018 | J Fr Ophtalmol | pmid:29567021 |
| Ekici Günay N et al. | Administration of Extract (EGb761) Alone and in Combination with FK506 Promotes Liver Regeneration in a Rat Model of Partial Hepatectomy. | 2018 | Balkan Med J | pmid:29553465 |
| Zhang X et al. | Current progress of tacrolimus dosing in solid organ transplant recipients: Pharmacogenetic considerations. | 2018 | Biomed. Pharmacother. | pmid:29550633 |
| Komine N et al. | Influence of CYP3A5 genetic differences in tacrolimus on quantitative interstitial fibrosis and long-term graft function in kidney transplant recipients. | 2018 | Int. Immunopharmacol. | pmid:29550576 |
| Kagaya H et al. | Prediction of Tacrolimus Exposure by CYP3A5 Genotype and Exposure of Co-Administered Everolimus in Japanese Renal Transplant Recipients. | 2018 | Int J Mol Sci | pmid:29547545 |
| Yamada R et al. | A case of duodenal malignant lymphoma presenting as acute pancreatitis: systemic lupus erythematosus and immunosuppressive therapy as risk factors. | 2018 | Clin J Gastroenterol | pmid:29546569 |
| Shi D et al. | CYP3A4 and GCK genetic polymorphisms are the risk factors of tacrolimus-induced new-onset diabetes after transplantation in renal transplant recipients. | 2018 | Eur. J. Clin. Pharmacol. | pmid:29546446 |
| Qin X et al. | Multi-center Performance Evaluations of Tacrolimus and Cyclosporine Electrochemiluminescence Immunoassays in the Asia-Pacific Region. | 2018 | Ann Lab Med | pmid:29214751 |
| Wan Q et al. | Therapeutic Effect of 0.1% Tacrolimus Eye Drops in the Tarsal Form of Vernal Keratoconjunctivitis. | 2018 | Ophthalmic Res. | pmid:28803239 |
| Fu Q et al. | Risk Factors for Acute Rejection After Deceased Donor Kidney Transplantation in China. | 2018 | Transplant. Proc. | pmid:30316380 |
| Konno O et al. | Early Outcomes of Living-Donor Kidney Transplantation With Immunosuppression Therapy Induction With Tacrolimus Extended-Release: A Comparison With Cyclosporine. | 2018 | Transplant. Proc. | pmid:30316378 |
| Tsujimura K et al. | Effect of Influenza Vaccine in Patients With Kidney Transplant. | 2018 | Transplant. Proc. | pmid:30316375 |
| Yu M et al. | Pharmacokinetics, Pharmacodynamics and Pharmacogenetics of Tacrolimus in Kidney Transplantation. | 2018 | Curr. Drug Metab. | pmid:29380698 |
| Kim JH et al. | Increased Exposure of Tacrolimus by Co-administered Mycophenolate Mofetil: Population Pharmacokinetic Analysis in Healthy Volunteers. | 2018 | Sci Rep | pmid:29374217 |
| Xia T et al. | Targeted metabolomic analysis of 33 amino acids and biogenic amines in human urine by ion-pairing HPLC-MS/MS: Biomarkers for tacrolimus nephrotoxicity after renal transplantation. | 2018 | Biomed. Chromatogr. | pmid:29369388 |
| Song JL et al. | Higher tacrolimus blood concentration is related to increased risk of post-transplantation diabetes mellitus after living donor liver transplantation. | 2018 | Int J Surg | pmid:29360611 |
| Charnaya O et al. | Results of early treatment for de novo donor-specific antibodies in pediatric kidney transplant recipients in a cross-sectional and longitudinal cohort. | 2018 | Pediatr Transplant | pmid:29356221 |
| Yamada K et al. | Correlation between disease activity and serum ferritin in clinically amyopathic dermatomyositis with rapidly-progressive interstitial lung disease: a case report. | 2018 | BMC Res Notes | pmid:29338781 |