| MeSH term | MeSH ID | Detail |
|---|---|---|
| Scorpion Stings | D065008 | 1 associated lipids |
| Drug-Related Side Effects and Adverse Reactions | D064420 | 3 associated lipids |
| Retrognathia | D063173 | 1 associated lipids |
| End Stage Liver Disease | D058625 | 1 associated lipids |
| Candidiasis, Invasive | D058365 | 2 associated lipids |
| Acute Kidney Injury | D058186 | 34 associated lipids |
| Thrombotic Microangiopathies | D057049 | 1 associated lipids |
| Central Serous Chorioretinopathy | D056833 | 1 associated lipids |
| Leukoencephalopathies | D056784 | 3 associated lipids |
| Netherton Syndrome | D056770 | 1 associated lipids |
| Latent Tuberculosis | D055985 | 1 associated lipids |
| Invasive Pulmonary Aspergillosis | D055744 | 1 associated lipids |
| Keratosis, Actinic | D055623 | 3 associated lipids |
| Multiple Pulmonary Nodules | D055613 | 2 associated lipids |
| Pancreatitis, Graft | D055589 | 1 associated lipids |
| Failed Back Surgery Syndrome | D055111 | 3 associated lipids |
| Primary Graft Dysfunction | D055031 | 1 associated lipids |
| Idiopathic Interstitial Pneumonias | D054988 | 1 associated lipids |
| Dendritic Cell Sarcoma, Interdigitating | D054739 | 1 associated lipids |
| Precursor Cell Lymphoblastic Leukemia-Lymphoma | D054198 | 10 associated lipids |
| Posterior Leukoencephalopathy Syndrome | D054038 | 1 associated lipids |
| Dysuria | D053159 | 1 associated lipids |
| Nocturia | D053158 | 1 associated lipids |
| Delayed Graft Function | D051799 | 2 associated lipids |
| Renal Insufficiency | D051437 | 8 associated lipids |
| Lymphohistiocytosis, Hemophagocytic | D051359 | 1 associated lipids |
| Granulomatosis, Orofacial | D051261 | 2 associated lipids |
| Atherosclerosis | D050197 | 85 associated lipids |
| Dyslipidemias | D050171 | 7 associated lipids |
| Diabetes Complications | D048909 | 4 associated lipids |
| Hepatic Insufficiency | D048550 | 1 associated lipids |
| Colitis, Collagenous | D046729 | 1 associated lipids |
| Protoporphyria, Erythropoietic | D046351 | 1 associated lipids |
| Coproporphyria, Hereditary | D046349 | 1 associated lipids |
| Ileus | D045823 | 3 associated lipids |
| Intestinal Volvulus | D045822 | 1 associated lipids |
| Cholecystolithiasis | D041761 | 2 associated lipids |
| Mastocytosis, Cutaneous | D034701 | 1 associated lipids |
| Hypoalbuminemia | D034141 | 1 associated lipids |
| Hyperuricemia | D033461 | 4 associated lipids |
| Papillomavirus Infections | D030361 | 4 associated lipids |
| Denys-Drash Syndrome | D030321 | 1 associated lipids |
| Pulmonary Disease, Chronic Obstructive | D029424 | 16 associated lipids |
| Polyomavirus Infections | D027601 | 1 associated lipids |
| Coronary Stenosis | D023921 | 6 associated lipids |
| Lacerations | D022125 | 1 associated lipids |
| Brachial Plexus Neuritis | D020968 | 2 associated lipids |
| Neuroaspergillosis | D020953 | 2 associated lipids |
| Hypoxia-Ischemia, Brain | D020925 | 22 associated lipids |
| Central Nervous System Viral Diseases | D020805 | 1 associated lipids |
| Intracranial Thrombosis | D020767 | 2 associated lipids |
| Parkinsonian Disorders | D020734 | 20 associated lipids |
| Nervous System Autoimmune Disease, Experimental | D020721 | 3 associated lipids |
| Stroke | D020521 | 32 associated lipids |
| Brain Infarction | D020520 | 17 associated lipids |
| Peroneal Neuropathies | D020427 | 1 associated lipids |
| Sciatic Neuropathy | D020426 | 13 associated lipids |
| Osteoarthritis, Knee | D020370 | 13 associated lipids |
| Paraneoplastic Syndromes, Nervous System | D020361 | 1 associated lipids |
| Hypertensive Encephalopathy | D020343 | 1 associated lipids |
| Migraine with Aura | D020325 | 1 associated lipids |
| Autoimmune Diseases of the Nervous System | D020274 | 1 associated lipids |
| Neurotoxicity Syndromes | D020258 | 34 associated lipids |
| Ventricular Remodeling | D020257 | 28 associated lipids |
| Infarction, Middle Cerebral Artery | D020244 | 35 associated lipids |
| Optic Nerve Injuries | D020221 | 4 associated lipids |
| Facial Nerve Injuries | D020220 | 1 associated lipids |
| Trauma, Nervous System | D020196 | 2 associated lipids |
| Nocturnal Myoclonus Syndrome | D020189 | 1 associated lipids |
| Sleep Apnea, Central | D020182 | 1 associated lipids |
| Citrullinemia | D020159 | 1 associated lipids |
| Hepatopulmonary Syndrome | D020065 | 1 associated lipids |
| Epstein-Barr Virus Infections | D020031 | 3 associated lipids |
| Genetic Predisposition to Disease | D020022 | 24 associated lipids |
| Miller Fisher Syndrome | D019846 | 1 associated lipids |
| Hepatitis C, Chronic | D019698 | 12 associated lipids |
| Hepatitis B, Chronic | D019694 | 4 associated lipids |
| Hepatitis, Autoimmune | D019693 | 1 associated lipids |
| Neurodegenerative Diseases | D019636 | 32 associated lipids |
| Intracranial Hypertension | D019586 | 4 associated lipids |
| Dermatitis, Perioral | D019557 | 4 associated lipids |
| Pouchitis | D019449 | 3 associated lipids |
| Endotoxemia | D019446 | 27 associated lipids |
| Oral Ulcer | D019226 | 1 associated lipids |
| Gingival Overgrowth | D019214 | 7 associated lipids |
| Fasciitis, Necrotizing | D019115 | 1 associated lipids |
| Postoperative Hemorrhage | D019106 | 7 associated lipids |
| Multiple Endocrine Neoplasia Type 2a | D018813 | 1 associated lipids |
| Anemia, Iron-Deficiency | D018798 | 6 associated lipids |
| Encephalitis, Viral | D018792 | 3 associated lipids |
| Hypoplastic Left Heart Syndrome | D018636 | 1 associated lipids |
| Cryptogenic Organizing Pneumonia | D018549 | 3 associated lipids |
| Ventricular Dysfunction, Left | D018487 | 33 associated lipids |
| Lichen Sclerosus et Atrophicus | D018459 | 2 associated lipids |
| Vasculitis, Leukocytoclastic, Cutaneous | D018366 | 5 associated lipids |
| Hutchinson's Melanotic Freckle | D018327 | 2 associated lipids |
| Angiofibroma | D018322 | 2 associated lipids |
| Cervical Intraepithelial Neoplasia | D018290 | 1 associated lipids |
| Seminoma | D018239 | 2 associated lipids |
| Smooth Muscle Tumor | D018235 | 1 associated lipids |
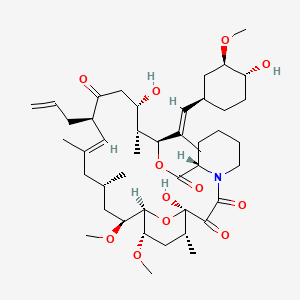
tacrolimus
Tacrolimus is a lipid of Polyketides (PK) class. Tacrolimus is associated with abnormalities such as Renal glomerular disease. The involved functions are known as inhibitors, Fungicidal activity, Metabolic Inhibition, Excretory function and Dephosphorylation. Tacrolimus often locates in Hepatic, Mitochondrial matrix and Inner mitochondrial membrane. The associated genes with Tacrolimus are RHOA gene and BGN gene.
Cross Reference
Introduction
To understand associated biological information of tacrolimus, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with tacrolimus?
tacrolimus is suspected in Renal glomerular disease, Candidiasis, Mycoses, PARKINSON DISEASE, LATE-ONSET, Morphologically altered structure, Skin Diseases, Infectious and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (2)
- Am. J. Physiol. Renal Physiol. (1)
- Drug Metab. Dispos. (1)
- Others (1)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with tacrolimus
PubChem Associated disorders and diseases
What pathways are associated with tacrolimus
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with tacrolimus?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with tacrolimus?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with tacrolimus?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with tacrolimus?
Related references are published most in these journals:
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with tacrolimus?
There are no associated biomedical information in the current reference collection.
NCBI Entrez Crosslinks
All references with tacrolimus
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Moon BJ et al. | Effect of chronic rhinosinusitis on liver transplant patients. | 2009 Sep-Oct | Am J Rhinol Allergy | pmid:19807981 |
| Shin JH et al. | The effect of topical FK506 (tacrolimus) in a mouse model of allergic rhinitis. | 2012 Mar-Apr | Am J Rhinol Allergy | pmid:22487280 |
| Vearrier D et al. | Mutism and persistent dysarthria due to tacrolimus-based immunosuppression following allogeneic liver transplantation. | 2011 | Am J Ther | pmid:20535006 |
| Yang A and Wang B | Sirolimus versus tacrolimus in kidney transplant recipients receiving mycophenolate mofetil and steroids: focus on acute rejection, patient and graft survival. | Am J Ther | pmid:23921809 | |
| Pariser D | Topical corticosteroids and topical calcineurin inhibitors in the treatment of atopic dermatitis: focus on percutaneous absorption. | 2009 May-Jun | Am J Ther | pmid:19262357 |
| Sathyan S et al. | Prevention of recurrent episodes of rhabdomyolysis with tacrolimus in a transplant recipient with myopathy. | Am J Ther | pmid:23429166 | |
| Liu JY et al. | Tacrolimus Versus Cyclosporine as Primary Immunosuppressant After Renal Transplantation: A Meta-Analysis and Economics Evaluation. | Am J Ther | pmid:25299636 | |
| Haroon N et al. | Tacrolimus Toxicity With Minimal Clinical Manifestations: A Case Report and Literature Review. | Am J Ther | pmid:25730156 | |
| Nunokawa T et al. | Late-onset scleroderma renal crisis induced by tacrolimus and prednisolone: a case report. | Am J Ther | pmid:22836123 | |
| Liu JY et al. | Sirolimus Versus Tacrolimus as Primary Immunosuppressant After Renal Transplantation: A Meta-Analysis and Economics Evaluation. | Am J Ther | pmid:25569597 | |
| Cohen SM | Current immunosuppression in liver transplantation. | 2002 Mar-Apr | Am J Ther | pmid:11897926 |
| Yousuf Bhat Z et al. | Colchicine-Induced Myopathy in a Tacrolimus-Treated Renal Transplant Recipient: Case Report and Literature Review. | Am J Ther | pmid:24732905 | |
| Azizian M et al. | Augmentation of ischemia/reperfusion injury to endothelial cells by cyclosporin A. | 2004 | Am Surg | pmid:15156953 |
| Henderson CN et al. | Continuous Abdominal Irrigation for Treatment of Tertiary Peritonitis in the Immunosuppressed Patient after Solid Organ Transplant: A Novel Approach. | 2017 | Am Surg | pmid:28424115 |
| Rojas-GarcÃa P et al. | Breast fibroadenomas associated with immunosuppressive drugs. | 2010 | Am Surg | pmid:21418766 |
| Kodama M et al. | FK506 therapy of experimental autoimmune myocarditis after onset of the disease. | 1993 | Am. Heart J. | pmid:7504393 |
| Chieffo A et al. | Histopathology of clinical coronary restenosis in drug-eluting versus bare metal stents. | 2009 | Am. J. Cardiol. | pmid:19962471 |
| Chang RK et al. | Marked left ventricular hypertrophy in children on tacrolimus (FK506) after orthotopic liver transplantation. | 1998 | Am. J. Cardiol. | pmid:9604971 |
| Klauss V et al. | Cyclosporine versus tacrolimus (FK 506) for prevention of cardiac allograft vasculopathy. | 2000 | Am. J. Cardiol. | pmid:10955391 |
| Herzberg GZ et al. | Usefulness of tacrolimus versus cyclosporine after pediatric heart transplantation. | 1998 | Am. J. Cardiol. | pmid:9723652 |
| Hisamura F et al. | Synergistic effect of green tea polyphenols on their protection against FK506-induced cytotoxicity in renal cells. | 2008 | Am. J. Chin. Med. | pmid:18543393 |
| Chung SY et al. | Ginkgo biloba leaf extract (EGb761) combined with neuroprotective agents reduces the infarct volumes of gerbil ischemic brain. | 2006 | Am. J. Chin. Med. | pmid:17080546 |
| Stickle DF et al. | Effects of sterilizing gamma irradiation on bloodspot newborn screening tests and whole blood cyclosporine and tacrolimus measurements. | 2003 | Am. J. Clin. Pathol. | pmid:12580001 |
| Wang E et al. | Pseudo-Pelger-Huët anomaly induced by medications: a clinicopathologic study in comparison with myelodysplastic syndrome-related pseudo-Pelger-Huët anomaly. | 2011 | Am. J. Clin. Pathol. | pmid:21228370 |
| Burke MT et al. | Expression of Bcl-xL and Mcl-1 in the nonmelanoma skin cancers of renal transplant recipients. | 2015 | Am. J. Clin. Pathol. | pmid:25780003 |
| Lower DR et al. | Comparison of CEDIA FK506 assay with HPLC/MS/MS in a large cohort of pediatric patients. | 2013 | Am. J. Clin. Pathol. | pmid:23690122 |
| Rudi J et al. | Prevalence of serum antibodies to Helicobacter pylori and to CagA protein in liver transplant recipients. | 1997 | Am. J. Gastroenterol. | pmid:9317070 |
| Van Thiel DH et al. | Tacrolimus (FK 506), a treatment for primary sclerosing cholangitis: results of an open-label preliminary trial. | 1995 | Am. J. Gastroenterol. | pmid:7532912 |
| Baumgart DC et al. | Tacrolimus is safe and effective in patients with severe steroid-refractory or steroid-dependent inflammatory bowel disease--a long-term follow-up. | 2006 | Am. J. Gastroenterol. | pmid:16573777 |
| Sandborn WJ | Preliminary report on the use of oral tacrolimus (FK506) in the treatment of complicated proximal small bowel and fistulizing Crohn's disease. | 1997 | Am. J. Gastroenterol. | pmid:9149205 |
| Van Thiel DH et al. | Tacrolimus: a potential new treatment for autoimmune chronic active hepatitis: results of an open-label preliminary trial. | 1995 | Am. J. Gastroenterol. | pmid:7537444 |
| Fellermann K et al. | Steroid-unresponsive acute attacks of inflammatory bowel disease: immunomodulation by tacrolimus (FK506). | 1998 | Am. J. Gastroenterol. | pmid:9772045 |
| Nara M et al. | Effect of oral itraconazole on the pharmacokinetics of tacrolimus in a hematopoietic stem cell transplant recipient with CYP3A5*3/*3. | 2010 | Am. J. Hematol. | pmid:20568249 |
| Lekakis LJ et al. | BK virus nephropathy after allogeneic stem cell transplantation: a case report and literature review. | 2009 | Am. J. Hematol. | pmid:19208419 |
| Hammerstrom AE et al. | Tacrolimus-associated posterior reversible encephalopathy syndrome in hematopoietic allogeneic stem cell transplantation. | 2013 | Am. J. Hematol. | pmid:23460378 |
| Abdel-Azim H et al. | Unrelated donor hematopoietic stem cell transplantation for the treatment of non-malignant genetic diseases: An alemtuzumab based regimen is associated with cure of clinical disease; earlier clearance of alemtuzumab may be associated with graft rejection. | 2015 | Am. J. Hematol. | pmid:26242764 |
| Uehara T et al. | Successful control of Epstein-Barr virus (EBV)-infected cells by allogeneic nonmyeloablative stem cell transplantation in a patient with the lethal form of chronic active EBV infection. | 2004 | Am. J. Hematol. | pmid:15282671 |
| Nakamae H et al. | Risk factor analysis for thrombotic microangiopathy after reduced-intensity or myeloablative allogeneic hematopoietic stem cell transplantation. | 2006 | Am. J. Hematol. | pmid:16755559 |
| Bolaños-Meade J et al. | Lymphocytic pneumonitis as the manifestation of acute graft-versus-host disease of the lung. | 2005 | Am. J. Hematol. | pmid:15929116 |
| Ninan MJ and Datta YH | Post-transplant lymphoproliferative disorder presenting as multiple myeloma. | 2010 | Am. J. Hematol. | pmid:20578201 |
| Mach-Pascual S et al. | Microangiopathic hemolytic anemia complicating FK506 (tacrolimus) therapy. | 1996 | Am. J. Hematol. | pmid:8701950 |
| Uehara T et al. | A successful second unrelated BMT (UBMT) from a different unrelated donor to treat ALL that relapsed after the initial UBMT. | 2002 | Am. J. Hematol. | pmid:12221672 |
| Cohen DL et al. | Pulse wave analysis to assess vascular compliance changes in stable renal transplant recipients. | 2004 | Am. J. Hypertens. | pmid:15001192 |
| Zhang W and Victor RG | Calcineurin inhibitors cause renal afferent activation in rats: a novel mechanism of cyclosporine-induced hypertension. | 2000 | Am. J. Hypertens. | pmid:10981550 |
| Taler SJ et al. | Loss of nocturnal blood pressure fall after liver transplantation during immunosuppressive therapy. | 1995 | Am. J. Hypertens. | pmid:7544983 |
| Rostaing L et al. | Novel Once-Daily Extended-Release Tacrolimus Versus Twice-Daily Tacrolimus in De Novo Kidney Transplant Recipients: Two-Year Results of Phase 3, Double-Blind, Randomized Trial. | 2016 | Am. J. Kidney Dis. | pmid:26717860 |
| van Duijnhoven EM et al. | A late episode of post-transplant diabetes mellitus during active hepatitis C infection in a renal allograft recipient using tacrolimus. | 2002 | Am. J. Kidney Dis. | pmid:12087579 |
| Moes AD et al. | Chlorthalidone Versus Amlodipine for Hypertension in Kidney Transplant Recipients Treated With Tacrolimus: A Randomized Crossover Trial. | 2017 | Am. J. Kidney Dis. | pmid:28259499 |
| Soi V et al. | Altered mental status in a kidney transplant recipient receiving tacrolimus. | 2008 | Am. J. Kidney Dis. | pmid:18155524 |
| Reese PP et al. | Automated Reminders and Physician Notification to Promote Immunosuppression Adherence Among Kidney Transplant Recipients: A Randomized Trial. | 2017 | Am. J. Kidney Dis. | pmid:27940063 |