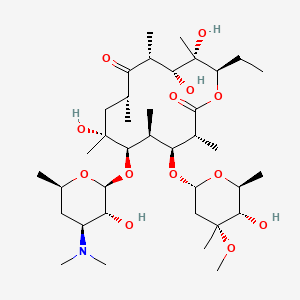
erythromycin
erythromycin is a lipid of Polyketides (PK) class. Erythromycin is associated with abnormalities such as Systemic Inflammatory Response Syndrome, Pneumonia, Infection, Pneumococcal Infections and Exanthema. The involved functions are known as Pharmacodynamics, Sterility, Agent, Drug Kinetics and Adjudication. Erythromycin often locates in Blood, peritoneal, Extracellular, Ribosomes and apicoplast. The associated genes with erythromycin are P4HTM gene, SLC33A1 gene, FAM3B gene, Operon and Homologous Gene. The related lipids are Hydroxytestosterones, Steroids, Propionate, Mycolic Acids and campesterol. The related experimental models are Mouse Model and Knock-out.
Cross Reference
Introduction
To understand associated biological information of erythromycin, we collected biological information of abnormalities, associated pathways, cellular/molecular locations, biological functions, related genes/proteins, lipids and common seen animal/experimental models with organized paragraphs from literatures.
What diseases are associated with erythromycin?
erythromycin is suspected in Pneumonia, Infection, Gonorrhea, Cystic Fibrosis, Respiratory Tract Infections, Influenza and other diseases in descending order of the highest number of associated sentences.
Related references are mostly published in these journals:
- Antimicrob. Agents Chemother. (35)
- J. Antimicrob. Chemother. (18)
- Clin. Infect. Dis. (2)
- Others (29)
| Disease | Cross reference | Weighted score | Related literature |
|---|
Possible diseases from mapped MeSH terms on references
We collected disease MeSH terms mapped to the references associated with erythromycin
PubChem Associated disorders and diseases
What pathways are associated with erythromycin
There are no associated biomedical information in the current reference collection.
PubChem Biomolecular Interactions and Pathways
Link to PubChem Biomolecular Interactions and PathwaysWhat cellular locations are associated with erythromycin?
Visualization in cellular structure
Associated locations are in red color. Not associated locations are in black.
Related references are published most in these journals:
- Antimicrob. Agents Chemother. (20)
- J. Antimicrob. Chemother. (9)
- Drug Metab. Dispos. (2)
- Others (20)
| Location | Cross reference | Weighted score | Related literatures |
|---|
What functions are associated with erythromycin?
Related references are published most in these journals:
| Function | Cross reference | Weighted score | Related literatures |
|---|
What lipids are associated with erythromycin?
Related references are published most in these journals:
| Lipid concept | Cross reference | Weighted score | Related literatures |
|---|
What genes are associated with erythromycin?
Related references are published most in these journals:
- Antimicrob. Agents Chemother. (19)
- J. Antimicrob. Chemother. (10)
- Drug Metab. Dispos. (5)
- Others (29)
| Gene | Cross reference | Weighted score | Related literatures |
|---|
What common seen animal models are associated with erythromycin?
Mouse Model
Mouse Model are used in the study 'In vitro and in vivo activities of macrolide derivatives against Mycobacterium tuberculosis.' (Falzari K et al., 2005) and Mouse Model are used in the study 'Activity of ABT-773 against Mycobacterium avium complex in the beige mouse model.' (Cynamon MH et al., 2000).
Knock-out
Knock-out are used in the study 'Functional expression and comparative characterization of nine murine cytochromes P450 by fluorescent inhibition screening.' (McLaughlin LA et al., 2008).
Related references are published most in these journals:
| Model | Cross reference | Weighted score | Related literatures |
|---|
NCBI Entrez Crosslinks
All references with erythromycin
Download all related citations| Authors | Title | Published | Journal | PubMed Link |
|---|---|---|---|---|
| Kamio K and Azuma A | Diffuse panbronchiolitis: A fine road from the discovery of a disease to the establishment of treatment. | 2018 | Respir Investig | pmid:30049592 |
| Young N et al. | Integrated point-of-care testing (POCT) of HIV, syphilis, malaria and anaemia in antenatal clinics in western Kenya: A longitudinal implementation study. | 2018 | PLoS ONE | pmid:30028852 |
| Dos Santos JFS et al. | In vitro e in silico evaluation of the inhibition of Staphylococcus aureus efflux pumps by caffeic and gallic acid. | 2018 | Comp. Immunol. Microbiol. Infect. Dis. | pmid:30017074 |
| Russo N et al. | Enterococcus spp. in Ragusano PDO and Pecorino Siciliano cheese types: A snapshot of their antibiotic resistance distribution. | 2018 | Food Chem. Toxicol. | pmid:30009890 |
| Papagiannitsis CC et al. | First Description in Greece of mphC-Positive Staphylococci Causing Subclinical Mastitis in Ewes. | 2018 | Microb. Drug Resist. | pmid:29489448 |
| Peng J et al. | Blue-light photoelectrochemical sensor based on nickel tetra-amined phthalocyanine-graphene oxide covalent compound for ultrasensitive detection of erythromycin. | 2018 | Biosens Bioelectron | pmid:29428591 |
| Akoachere JTK et al. | Bacterial and parasitic contaminants of salad vegetables sold in markets in Fako Division, Cameroon and evaluation of hygiene and handling practices of vendors. | 2018 | BMC Res Notes | pmid:29409524 |
| Tatsuno I et al. | Functional Predominance of msr(D), Which Is More Effective as mef(A)-Associated Than mef(E)-Associated, Over mef(A)/mef(E) in Macrolide Resistance in Streptococcus pyogenes. | 2018 | Microb. Drug Resist. | pmid:29406792 |
| Hawkins PA et al. | Cross-resistance to lincosamides, streptogramins A and pleuromutilins in Streptococcus agalactiae isolates from the USA. | 2017 | J. Antimicrob. Chemother. | pmid:28333320 |
| Demczuk WHB et al. | Phylogenetic analysis of emergent Streptococcus pneumoniae serotype 22F causing invasive pneumococcal disease using whole genome sequencing. | 2017 | PLoS ONE | pmid:28531208 |
| Cheled-Shoval S et al. | From Cell to Beak: In-Vitro and In-Vivo Characterization of Chicken Bitter Taste Thresholds. | 2017 | Molecules | pmid:28513558 |
| Sato T et al. | Mycoplasma bovis isolates from dairy calves in Japan have less susceptibility than a reference strain to all approved macrolides associated with a point mutation (G748A) combined with multiple species-specific nucleotide alterations in 23S rRNA. | 2017 | Microbiol. Immunol. | pmid:28504455 |
| Wozniak A et al. | Importance of adhesins in the recurrence of pharyngeal infections caused by Streptococcus pyogenes. | 2017 | J. Med. Microbiol. | pmid:28463664 |
| Pergola S et al. | Genetic diversity and antimicrobial resistance profiles of Campylobacter coli and Campylobacter jejuni isolated from broiler chicken in farms and at time of slaughter in central Italy. | 2017 | J. Appl. Microbiol. | pmid:28194914 |
| Huang YW et al. | Overexpression of SmeDEF Efflux Pump Decreases Aminoglycoside Resistance in Stenotrophomonas maltophilia. | 2017 | Antimicrob. Agents Chemother. | pmid:28193669 |
| Ge LL et al. | [Antibiotic resistance analysis of isolates from the hospitalized children in Shanxi Children's Hospital from 2012 to 2014]. | 2017 | Zhonghua Er Ke Za Zhi | pmid:28173648 |
| Giguère S | Treatment of Infections Caused by Rhodococcus equi. | 2017 | Vet. Clin. North Am. Equine Pract. | pmid:28161038 |
| Wang Y et al. | Evaluation of a series of 2-napthamide derivatives as inhibitors of the drug efflux pump AcrB for the reversal of antimicrobial resistance. | 2017 | Bioorg. Med. Chem. Lett. | pmid:28129976 |
| Kassem II et al. | Antimicrobial-Resistant Campylobacter in Organically and Conventionally Raised Layer Chickens. | 2017 | Foodborne Pathog. Dis. | pmid:27768387 |
| Michael-Kordatou I et al. | On the capacity of ozonation to remove antimicrobial compounds, resistant bacteria and toxicity from urban wastewater effluents. | 2017 | J. Hazard. Mater. | pmid:26947803 |